The pursuit of facial harmony and congruence with one’s deeply held gender identity is a profound journey for many individuals. Gezichtsfeminisering Surgery (FFS) stands as a cornerstone in this transformative process, meticulously reshaping facial features to align with a more feminine aesthetic. However, the path to achieving optimal results is not always linear. Despite advancements in surgical technieken and a growing understanding of gender-affirming care, a subset of patients may find themselves seeking revision FFS to address outcomes that, for various reasons, fall short of their expectations or surgical goals. This specialized area of aesthetic surgery is not merely about correcting “mistakes” but about refining, enhancing, and often completing a patient’s vision for their facial appearance, ensuring it truly reflects their authentic self.
Revision FFS encompasses a complex array of surgical methodologies designed to correct suboptimal results from initial feminization procedures. These suboptimal outcomes can stem from a multitude of factors, including the inherent unpredictability of human healing, anatomical complexities that become more apparent post-operatively, or even the evolving aesthetic preferences of the individual over time. For instance, sometimes the initial surgical corrections may not have been extensive enough, leading to an “under-correction” where masculine features are still too prominent. Conversely, an “over-correction” could result in an unnatural or overly sculpted appearance. Asymmetry, visible scarring, or incomplete feminization in certain facial zones are also common drivers for individuals to overwegen a revision. The Feminization Center highlights that reasons for revision can include unnatural-looking results, asymmetry, visible scarring, incomplete results, and changes in aesthetic preferences (Feminization Center, n.d.). Similarly, Facialteam acknowledges that re-operations are common in FFS due to factors like lack of skill, professionalism, or poor aftercare, though they boast a low revision rate of 3% (Facialteam, n.d.).
The necessity for a specialized surgical approach in revision FFS is underscored by the unique challenges presented by previously operated tissues. Surgeons undertaking these procedures must navigate altered anatomical planes, scar tissue, and potentially compromised vascularity, all of which demand an advanced level of expertise, meticulous planning, and a nuanced understanding of facial aesthetics. The Ultimate FFS-revisie Guide by Dokter MFO emphasizes that surgeons performing redos may encounter unexpected circumstances such as asymmetrical scarring or adhesions, requiring detailed planning (Dr. MFO FFS Revision 2, 2024). This guide will delve into the intricate surgical methodologies and strategic considerations employed in advanced revision FFS, offering a detailed roadmap for understanding how surgeons address and correct less-than-optimal outcomes from prior procedures. We will explore the nuanced techniques applied to various facial regions, from the forehead and brow to the jaw, chin, nose, and midface, as well as strategies for managing soft tissue concerns and scars. Furthermore, we will emphasize the critical role of advanced diagnostic imaging, judicious graft selection, and the distinct recovery profile associated with revision cases. By providing a comprehensive, evidence-based analysis, this discourse aims to serve as an authoritative resource for individuals considering revision FFS, as well as for professionals seeking a deeper understanding of these intricate and highly specialized surgical interventions. The goal is not just to modify physical features but to achieve a profound sense of self-alignment and aesthetic harmony that significantly enhances an individual’s quality of life and confidence. The evolution of FFS has been marked by technological advancements in imaging, surgical tools, and materials, leading to minimally invasive techniques that reduce scarring and recovery time (The Spiegel Center, n.d.). This advanced landscape informs all aspects of revision FFS, making precise, patient-centered care more achievable than ever before. Understanding the interplay of surgical factors, patient physiology, evolving aesthetic goals, and unforeseen complications is paramount to approaching revision FFS with informed confidence, ultimately guiding patients toward their most authentic and harmonized facial presentation.
Inhoudsopgave
Advanced Revision FFS: Surgical Techniques for Correcting Suboptimal Outcomes
Forehead and Brow Revision
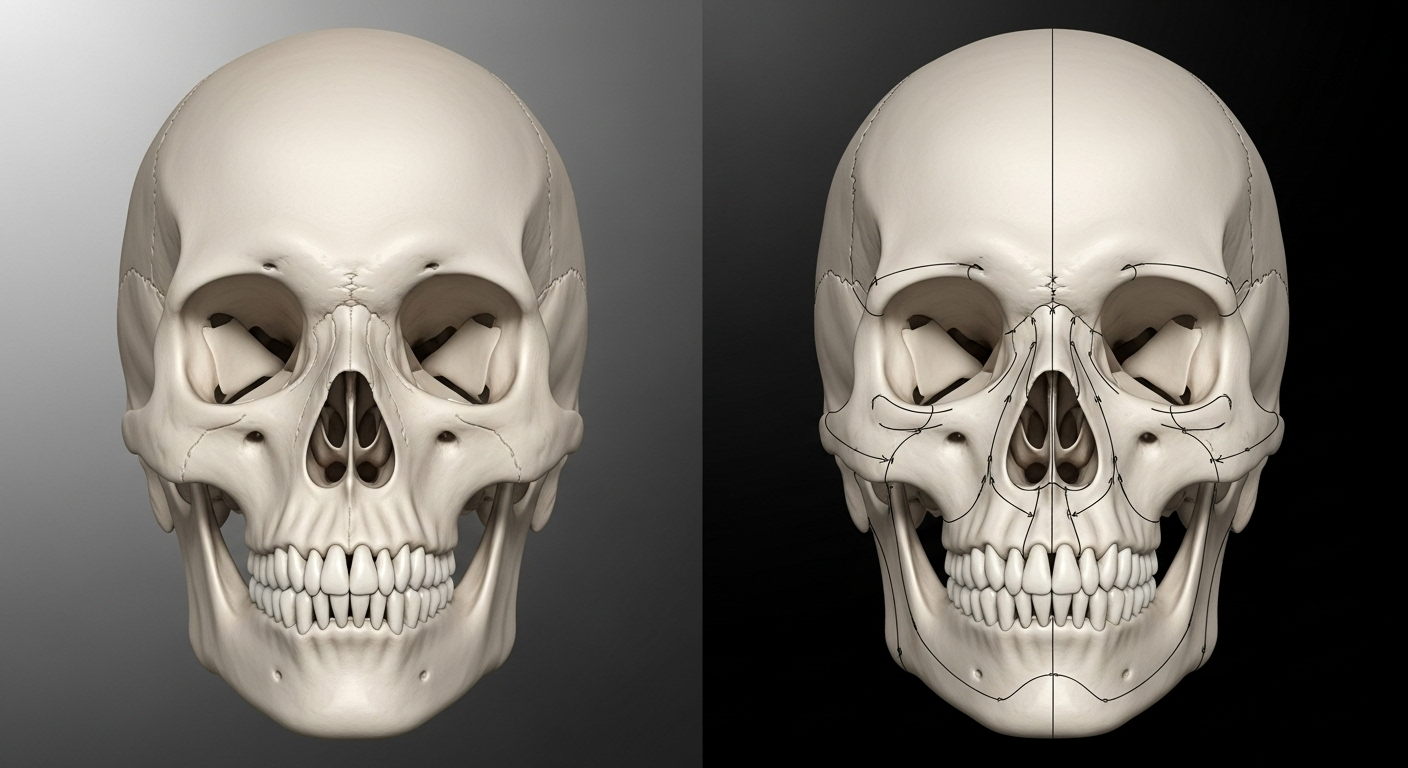
The forehead and brow region are paramount in determining perceived gender. Masculine foreheads typically feature a prominent brow bossing, a more defined ridge above the eyes, and often a higher or M-shaped hairline. Feminine foreheads, in contrast, are characterized by a smoother, more rounded contour and a lower, often oval-shaped hairline. Correcting suboptimal outcomes in this area during revision FFS demands exceptional precision, as the bone structure is fundamental to the overall facial impression.
One of the most frequent reasons for revision in the upper face is the **under-reduction of the brow bone**. If the initial surgery did not sufficiently reduce the supraorbital ridge, a noticeable prominence may persist, hindering the desired feminization. Revision techniques in such cases involve further burring or precise reshaping of the frontal bone to achieve a smoother, more effeminate contour. This can be a delicate procedure, as the thickness of the frontal bone varies, and excessive reduction carries risks. Dr. MFO highlights that under-reduction of the brow bone is a common reason for revision (Dr. MFO FFS Revision 1, 2025). The Gender Confirmation Center describes frontal sinus setback as a procedure that reduces or reshapes the brow bone to make the upper third of the face appear softer and less prominent (Gender Confirmation Center, n.d.).
Another significant concern requiring revision is the presence of **irregularities or depressions** on the forehead. These subtle imperfections can arise during the initial healing process, particularly following Type III cranioplasty procedures where a section of bone is removed, reshaped, and reattached. Minor bumps or depressions can become visible as swelling subsides. Revision strategies for these issues may involve targeted burring to smooth out bony irregularities. In select, more complex cases, vet enten or specialized bone cements can be employed to meticulously fill depressions and restore a seamless contour.
**Hairline irregularities or recessions** also frequently necessitate revision. An initial hairline advancement procedure might not have achieved the optimal shape or sufficient reduction of the forehead height, leaving an irregular or still-receding hairline that detracts from the overall feminine frame. Revision can involve further hairline advancement, often through careful scalp excision, to lower the hairline and create a more natural, rounded shape. Hair grafting can also be used in conjunction with advancement to increase density or refine the hairline’s aesthetic. The Gender Confirmation Center mentions hairline advancement (also known as hairline lowering) uses an incision around the forehead to reshape the hairline, focusing on rounding the corners of M-shaped hairlines and making the forehead appear shorter and more round (Gender Confirmation Center, n.d.).
**Brow asymmetry** can be another challenging issue. While sometimes related to soft tissue positioning, persistent brow asymmetry may indicate an underlying bony discrepancy that was not fully addressed. Revision in such instances can involve targeted bone work to re-balance the orbital rims or a more refined brow lift to ensure symmetry in eyebrow height and arch. Endoscopic methods are increasingly utilized to minimize scarring and improve precision in these delicate revisions (Dr. MFO FFS Revision 1, 2025).
The anatomical complexity of the forehead and brow, coupled with its central role in gender perception, makes revision procedures in this area particularly demanding. Surgeons must possess not only a deep understanding of craniofacial anatomy but also an artistic eye to sculpt a harmonious and natural-looking feminine contour. The importance of virtual surgical planning and 3D imaging in these cases cannot be overstated, as they allow for precise pre-operative assessment and detailed surgical strategy, mitigating potential pitfalls. Facialteam emphasizes detailed assessment and planning with patient input for predictable, safe, and precise results, which significantly reduces revision rates (Facialteam, n.d.). These tools are crucial for navigating the delicate balance between effective feminization and preserving structural integrity.

Jaw and Chin Revision
The lower third of the face, comprising the jaw and chin, plays a pivotal role in distinguishing masculine from feminine features. A typically masculine jawline is often characterized by a square, broad appearance with prominent angles, and a chin that can be tall and broad with significant projection. In contrast, feminine lower facial contours are generally softer, more tapered, and often present with a “V-shaped” or rounded chin. Revision FFS in this region frequently addresses concerns such as insufficient contouring, over-reduction, or the presence of bony irregularities and asymmetries that detract from the desired feminine aesthetic.
One of the primary drivers for revision is **insufficient jaw angle reduction**. If the initial mandibular angle shaving was conservative, or if bone regrowth occurs, the jawline may retain a masculine angularity. In these instances, revision involves further osteotomy—the surgical removal of bone—to achieve a softer, more tapered, and less prominent jawline. This requires meticulous planning to ensure symmetry and avoid over-reduction, which could lead to an unnatural or “pinched” appearance. The study by Gursky et al. on genioplasty in FFS highlights that masculine chins are typically taller and broader with more pronounced projection, while feminine chins are softer, less prominent, and sometimes V-shaped (Gursky et al., 2024). Jaw contouring aims to shave down the jaw and reshape the chin for a more narrow and softer look (Gender Confirmation Center, n.d.).
**Chin asymmetry or under-correction** after an initial genioplasty is another common reason for revision. The chin’s projection, width, and vertical height are critical for facial balance. If the initial procedure did not adequately reduce a prominent chin, or if it left an uneven contour, revision surgery can address these discrepancies. This may involve further bone reshaping to correct asymmetry, increase or decrease projection as desired, or refine the chin’s shape (e.g., to be more rounded or pointed). The review by Gursky et al. indicates that reduction genioplasty is the most common technique for feminizing the chin, with sliding genioplasty also detailed, often combined with bony burring for additional contouring (Gursky et al., 2024). Dr. MFO notes that revision for the chin can involve further bone reshaping to correct asymmetry, or to adjust projection or shape if the initial genioplasty was insufficient (Dr. MFO FFS Revision 1, 2025).
**Palpable irregularities** along the resected jawline or chin are also concerns that can lead to revision. These might manifest as small bumps, steps, or unevenness in the bone contour that become apparent upon palpation or visible under certain lighting. Revision surgery focuses on carefully burring or smoothing these areas to create a seamless and natural transition along the bone, enhancing both the tactile and visual smoothness of the lower face.
The technical complexities of jaw and chin revision are often heightened by the presence of existing scar tissue and altered soft tissue adherence. Surgeons must precisely re-osteotomize or burr bone while preserving critical anatomical structures such as nerves and blood vessels. Advanced imaging techniques, including 3D CT scans, are indispensable for pre-operative planning, enabling the chirurg to visualize the underlying bony architecture, assess previous osteotomie lines, and meticulously plan the corrective actions. Facialteam emphasizes that planning and experience significantly increase the likelihood of success in FFS and help address problems from previously incorrectly implemented operations (Facialteam, n.d.). Such detailed planning is crucial for achieving predictable, safe, and precise outcomes, especially in secondary procedures where the anatomical landscape has been altered. The objective is to achieve not just a reduction or reshaping, but a harmonious integration of the lower face with the overall feminized facial aesthetic, thereby contributing to a profound sense of self-alignment.
Nasal Revision (Rhinoplasty)
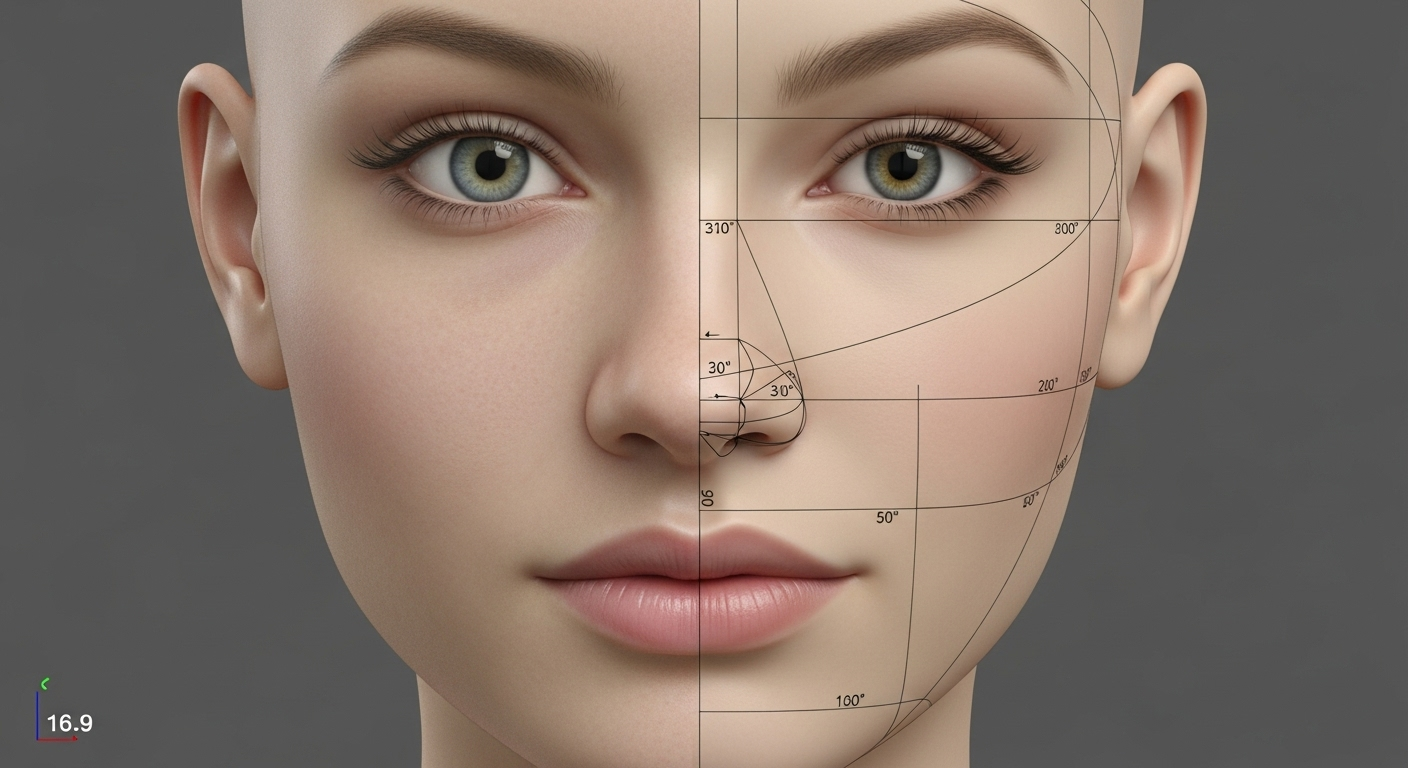
Nasal morphology is a crucial determinant of facial gender perception. Masculine noses often present with a broader bridge, a more prominent dorsal hump, and a less refined tip, typically projecting further from the face. Feminine noses, conversely, are generally characterized by a narrower, more delicate bridge, a subtle or absent dorsal hump, a refined and slightly upturned tip, and a harmonious relationship with other facial features. Revision neuscorrectie, following an initial Gezichtsfeminisatiechirurgie (FFS), is a highly intricate procedure that aims to correct aesthetic and sometimes functional shortcomings from the primary operation. Given the nose’s central position on the face and its complex cartilaginous and bony architecture, it is among the most frequently revised facial procedures.
One of the common reasons for revision is **persistent dorsal hump or width**. If the initial FFS rhinoplasty did not adequately reduce the bridge of the nose, a remaining masculine prominence or excessive width can be observed. Revision involves further precise bone and cartilage reduction to sculpt a smoother, more delicate nasal profile that integrates harmoniously with the feminized forehead and midface. This requires careful judgment to avoid over-resection, which can lead to an undesirable “scooped” or “pinched” appearance, a more challenging issue to correct. Allure Esthetic notes that a rhinoplasty is often chosen for revision if it was not adequately thinned, feminized, or supported, with many revisions occurring years after the initial procedure due to aging and facial changes (Allure Esthetic, n.d.). Dr. MFO also lists persistent dorsal hump or width as reasons for revision (Dr. MFO FFS Revision 1, 2025).
**Tip irregularities** are another frequent concern. The nasal tip is a complex area composed of delicate cartilages, and achieving a refined, slightly upturned, and symmetrical tip is a hallmark of feminizing rhinoplasty. If the initial surgery resulted in a tip that remains too bulbous, asymmetrical, or lacks adequate projection or rotation, revision may be necessary. Techniques often involve precise suturing of existing cartilages, or the use of cartilage grafts—often harvested from the septum, ear, or rib—to augment, reshape, and support the tip, creating a more delicate and defined aesthetic.
While primarily aesthetic, **breathing issues (functional revision)** can occasionally arise or persist after FFS rhinoplasty. Less commonly, an initial feminizing rhinoplasty might inadvertently lead to or exacerbate difficulties in nasal airflow. In such cases, revision focuses on addressing internal structural issues, such as septal deviations or collapse of the internal nasal valve, to improve respiratory function while simultaneously enhancing aesthetic outcomes.
**Asymmetry** of the nose, though often subtle and inherent in all faces, can become a noticeable concern after surgery. If a significant asymmetry of the nostrils, bridge, or tip develops or persists post-operatively, revision aims to improve overall nasal symmetry, contributing to a more balanced facial appearance. The Spiegel Center highlights that Dr. Spiegel was one of the first surgeons to perform lip lifts with rhinoplasty, indicating the integrated approach in facial feminization (The Spiegel Center, n.d.).
**Over-reduction**, while less common, is a particularly complex issue in revision rhinoplasty. If too much bone or cartilage was removed during the primary surgery, resulting in an overly “scooped” dorsal profile or a “pinched” tip, rebuilding the nasal structure often requires extensive cartilage grafting. This reconstructive aspect of revision rhinoplasty demands advanced surgical skill and artistry to restore natural contours and functional integrity.
Revision rhinoplasty is technically demanding due to the scar tissue from previous surgery, which can alter tissue elasticity and vascularity. Meticulous dissection, careful preservation of remaining cartilage, and strategic grafting are crucial for successful outcomes. Pre-operative 3D imaging is invaluable for assessing the existing nasal framework and planning precise corrective maneuvers. The goal of revision rhinoplasty is to achieve a refined, natural-looking nose that harmonizes with the feminized features of the entire face, contributing significantly to a patient’s confidence and perceived gender congruence.
Cheek and Midface Revision
The midface, particularly the cheeks, is a key region in defining facial femininity. Masculine midfaces tend to be flatter, with less pronounced cheekbones, while feminine midfaces often feature fuller, higher, and more rounded cheek contours, contributing to a softer, more youthful, and often heart-shaped facial outline. Revision FFS in the cheek and midface area primarily focuses on correcting volume discrepancies, adjusting implant placement or size, and addressing any irregularities that may have arisen from previous augmentation or contouring procedures.
One of the main objectives of midface revision is **correcting volume discrepancies**. If an initial fat grafting or implant procedure resulted in uneven volume distribution, or if there was insufficient augmentation to achieve the desired feminine fullness, revision can restore balance. This often involves additional **fat grafting**, where fat is harvested from another part of the body, processed, and meticulously injected into areas needing more volume. Fat grafting is particularly advantageous as it uses the patient’s own tissue, reducing the risk of rejection and providing natural-feeling results. However, fat graft survival can be variable, sometimes necessitating touch-ups (Dr. MFO FFS Revision 1, 2025). The Gender Confirmation Center notes that cheek augmentation can involve the use of wang implantaten, fillers, or analogous fat transfer (Gender Confirmation Center, n.d.).
For patients who underwent **cheek implant placement** in their primary surgery, revision may be required to adjust the placement or size of these implants. Implants that are incorrectly positioned can lead to asymmetry, an unnatural contour, or be palpable beneath the skin. Revision involves carefully repositioning existing implants, exchanging them for different sizes or shapes, or in some cases, removing them entirely if they are no longer desired or are causing complications. The complexity arises from navigating existing fibrous tissue around the implants and ensuring precise new placement for optimal aesthetic integration.
Another concern in midface revision is addressing **facial fat grafting irregularities**. While fat grafting is a versatile technique for adding volume, sometimes the grafted fat can settle unevenly, leading to small lumps, depressions, or an asymmetrical appearance. Revision for such irregularities might involve targeted massage, micro-liposuction of areas with excess fat, or additional, more carefully placed grafting to smooth contours. The Spiegel Center also notes that dermal fillers and fat grafting can be used to add volume to cheeks and lips for a more youthful and feminine look, and advancements in injectable treatments offer non-surgical options (The Spiegel Center, n.d.). This highlights a broader approach that may involve both surgical and non-surgical modalities in revision.
The midface is highly dynamic, influenced by expressions and the aging process. Therefore, revision considerations also account for how changes will integrate over time. The approach to midface revision is highly individualized, requiring a surgeon with a keen aesthetic eye and extensive experience in both soft tissue management and bone/implant adjustments. Pre-operative advanced imaging, such as 3D CT scans, assists in evaluating the underlying bone structure and the precise positioning of any previous implants or areas of fat grafting, allowing for meticulous planning. The overarching goal is to create a soft, rounded, and harmonized midface that contributes significantly to the feminized appearance, addressing any lingering sources of concern from previous procedures.
Soft Tissue Revisions
Beyond the foundational bony alterations, soft tissue procedures are integral to achieving a comprehensive feminine aesthetic in Facial Feminization Surgery (FFS). These elements, which include the skin, fat, muscles, and their collective drape, play a significant role in refining facial contours, improving texture, and managing visible signs of surgery. Revision FFS often extends to soft tissue adjustments, addressing issues such as persistent scarring, skin laxity, or inadequate soft tissue volume, which can all impact the final aesthetic outcome.
**Scar management techniques** are a critical component of soft tissue revisions. While FFS surgeons meticulously plan incisions to be as inconspicuous as possible—often hidden within the hairline or natural creases—some patients may still develop noticeable scars due to individual healing responses, genetic predispositions, or complications such as infection. Revision for unsightly scars can involve various methods, including:
- **Surgical scar revision:** This technique involves excising the existing scar and meticulously re-closing the incision with advanced suturing techniques to create a finer, less noticeable scar. This is particularly effective for wide, hypertrophic, or keloid scars, though careful patient selection and post-operative scar care are crucial. Allure Esthetic highlights that scar revision can correct unsightly scars (Allure Esthetic, n.d.).
- **Laser treatments:** Fractional laser resurfacing can improve scar texture, color, and overall appearance by stimulating collagen remodeling.
- **Microneedling:** This minimally invasive technique uses fine needles to create controlled micro-injuries, promoting collagen and elastin production to smooth and soften scars.
- **Corticosteroid injections:** For raised, hypertrophic, or keloid scars, targeted injections can help flatten and soften the tissue.
Addressing **residual soft tissue laxity** is another important aspect of soft tissue revisions. While bone reductions provide the structural framework for feminization, the overlying skin and soft tissues must redrape smoothly. In some cases, especially with significant bone reduction or in older patients, residual skin laxity or sagging can occur, leading to an aged or less refined appearance. Revision strategies may include:
- **Mini-facelift or neck lift procedures:** These involve excising excess skin and tightening the underlying fascial layers (SMAS) to create a smoother, more youthful contour in the lower face and neck.
- **Thread lifts:** Less invasive options, thread lifts can provide a temporary lift to sagging tissues, though their effects are generally less dramatic and long-lasting than surgical lifts.
- **Energy-based skin tightening:** Technologies like radiofrequency (RF) or ultrasound can stimulate collagen production to improve skin elasticity and tightness over time, offering a non-surgical approach to mild laxity. The Spiegel Center mentions minimally invasive techniques like Embrace (FaceTite or FaceTite to the neck with Morpheus8) for lifting skin through small incisions (The Spiegel Center, n.d.).
**Volume adjustments** in soft tissues, beyond those of the midface, may also be required. For instance, **lip lift revision** can be performed if the initial lift did not achieve the desired amount of upper lip eversion, or if there is a persistent long philtrum (distance between the nose and upper lip). Minor revisions might involve removing a small additional strip of skin at the base of the nose to further shorten the upper lip (Dr. MFO FFS Revision 1, 2025). Furthermore, if initial soft tissue augmentation with fillers or fat grafting in areas like the temples or periorbital region (around the eyes) was uneven or insufficient, additional augmentation can be performed to refine contours and restore youthful fullness. The Spiegel Center notes that non-surgical options with dermal fillers are available for soft tissue enhancements (The Spiegel Center, n.d.).
The success of soft tissue revisions relies heavily on the surgeon’s artistic judgment and experience in delicate tissue handling. The interplay between bone and soft tissue is crucial; therefore, revisions must consider both the underlying structure and the superficial drape to achieve a natural, harmonious, and enduring feminine result. Comprehensive patient assessment, realistic goal setting, and a multi-modal approach combining surgical and non-surgical techniques are often employed to optimize outcomes in soft tissue revision FFS.
Key Surgical Considerations in Revision FFS
Revision Facial Feminization Surgery (FFS) presents a distinct set of challenges that necessitate specialized surgical considerations beyond those of primary FFS. The altered anatomy, presence of scar tissue, and potential for compromised tissue integrity demand advanced planning, sophisticated techniques, and a profound understanding of facial aesthetics and healing dynamics. Addressing these unique aspects is crucial for achieving predictable and satisfying outcomes in secondary procedures.
1. The Role of Advanced Imaging and Virtual Surgical Planning
In revision FFS, accurate pre-operative assessment is paramount. Traditional 2D photographs and physical examinations provide valuable information, but **advanced 3D imaging, such as Computed Tomography (CT) scans with 3D reconstruction**, is indispensable. These scans offer an unprecedented view of the underlying bony architecture, allowing the surgeon to precisely map out existing bone reductions or augmentations, identify any residual prominences, and detect subtle asymmetries that may not be apparent externally. The review by Gursky et al. highlights that preoperative imaging and VSP are widely used, with CT scans with 3D reconstruction employed in 75% of included studies to enhance visualization and surgical planning (Gursky etal., 2024).
**Virtual Surgical Planning (VSP)**, a sophisticated digital tool, takes 3D imaging a step further. It allows surgeons to perform virtual osteotomies and contouring on a digital model of the patient’s face, simulating various surgical maneuvers and predicting their effects on both bone and soft tissue. This virtual rehearsal enables the surgeon to refine the surgical plan, optimize bone cuts, and design custom 3D-printed guides or plates for intraoperative precision. While VSP can be costly and time-consuming, it has been shown to improve accuracy, especially in complex cases like forehead reconstruction, and ensures that the revision addresses the patient’s precise aesthetic goals (Gursky et al., 2024). The Gender Confirmation Center advises considering facilities that use pre-surgery imaging like CT scans for planning (Allure Esthetic, n.d.). Facialteam emphasizes that their detailed assessment process with patient input and planning with 3D technology leads to predictable, safe, and precise results (Facialteam, n.d.).
2. Graft Selection (Bone/Cartilage) and Soft Tissue Management
In revision FFS, the need for **grafting materials** is often heightened due to potential over-resection in previous surgeries or the desire for augmentation.
- **Bone grafts:** Autologous bone (harvested from the patient’s own body, such as rib or calvarial bone) is often preferred for large volume augmentation or structural support, particularly in cases of over-reduced brow bones or chins. Synthetic bone substitutes can also be considered.
- **Cartilage grafts:** Autologous cartilage (typically from the nasal septum, ear, or rib) is invaluable for refining delicate structures like the nasal tip, reconstructing alar cartilages, or correcting minor contour irregularities in the brow or jaw.
The choice of graft material is critical, impacting long-term stability, integration, and overall aesthetic outcome.
**Soft tissue management** in revision FFS is particularly challenging. Prior surgery introduces scar tissue, which can alter tissue elasticity, vascularity, and the natural planes of dissection. This necessitates meticulous and careful surgical technique to avoid further scarring, nerve damage, or compromising blood supply. Techniques like targeted fat grafting (using the patient’s own fat) can be employed to camouflage irregularities, restore volume, and improve skin quality over previously operated areas (Dr. MFO FFS Revision 1, 2025). The Spiegel Center notes that soft tissue procedures are equally important and involve modifying skin, fat, and muscles (The Spiegel Center, n.d.).
3. Distinct Recovery Profile for Revision Cases
Patients undergoing revision FFS often experience a recovery that differs from their initial surgery.
- **Increased swelling and bruising:** Due to the presence of scar tissue and altered lymphatic drainage, swelling and bruising can be more pronounced and prolonged in revision cases. Patients need to be prepared for an extended period of post-operative edema.
- **Pain management:** While pain is manageable, the patient’s psychological state can influence their perception of discomfort.
- **Emotional impact:** Patients seeking revision often carry a heavier emotional burden due to dissatisfaction with previous results. Comprehensive psychological support and realistic expectation setting are crucial. The Feminization Center emphasizes that redo FFS can be an emotionally charged process, and open communication with the surgeon and a trusted support system are crucial (Feminization Center, n.d.).
- **Extended healing timeline:** Surgeons typically recommend waiting a minimum of 6-12 months, and often up to 18 months, after the initial FFS before considering revision. This allows for complete resolution of swelling and soft tissue settling, ensuring that any perceived irregularities are truly permanent and warrant further intervention (Dr. MFO FFS Revision 1, 2025; Allure Esthetic, n.d.).
In essence, key surgical considerations in revision FFS revolve around advanced diagnostic capabilities, strategic material selection, and a holistic understanding of the patient’s physical and emotional journey. The expertise of the surgeon in navigating these complexities is paramount to achieving transformative and enduring results.

Conclusie
The journey through Facial Feminization Surgery, and particularly the pursuit of revision FFS, underscores a profound commitment to achieving a true alignment between one’s inner self and outward presentation. While the initial FFS procedures represent a significant step toward gender affirmation for many, the reality of complex aesthetic interventions dictates that some individuals may require further refinement to fully realize their desired facial harmony. This detailed exploration into the methodologies and considerations of advanced revision FFS reveals not only the intricate technical demands of such surgeries but also the deeply personal and transformative impact they hold for patients.
We have traversed the nuanced landscape of revision across various facial zones, from the subtle yet impactful reshaping of the forehead and brow to the meticulous adjustments required for the jaw and chin. In the upper face, addressing under-reductions, irregularities, hairline concerns, and asymmetries necessitates precise bone work and often adjunctive soft tissue procedures, all aimed at fostering a smoother, more feminized contour. For the lower face, revision techniques delve into correcting insufficient jaw angle reductions, asymmetrical chins, and palpable bony irregularities, striving for a softer, tapered outline that complements the overall feminine aesthetic. Nasal revision, a particularly delicate undertaking, often corrects persistent dorsal humps, tip irregularities, and functional concerns, with advanced grafting techniques playing a critical role in structural and aesthetic refinement. The midface, with its emphasis on volume and contour, benefits from revisions that rectify discrepancies through targeted fat grafting or implant adjustments, ensuring a youthful and harmonious fullness. Finally, soft tissue revisions, including scar management and addressing skin laxity, are indispensable for perfecting the superficial elements and contributing to a seamless, natural-looking result.
The overarching theme in successful revision FFS is the integration of advanced diagnostic tools with exceptional surgical expertise and empathetic patient care. The indispensable role of 3D imaging and virtual surgical planning cannot be overstated, as these technologies provide surgeons with unparalleled insights into the underlying anatomy and the precision required for complex secondary alterations. Furthermore, the judicious selection and application of bone and cartilage grafts are fundamental to reconstructing and augmenting areas that may have been over-resected or require additional volume. However, the technical prowess must be balanced with a profound understanding of the distinct psychological and physiological recovery profile inherent in revision cases. Patients embarking on this second chapter of their surgical journey often bring with them a unique set of emotional considerations, necessitating comprehensive support and the setting of realistic expectations. Patience during the extended healing timeline, often 6 to 18 months, is crucial for allowing tissues to fully settle and for final results to emerge before definitive evaluation. The Feminization Center highlights the emotional journey of redo FFS, emphasizing the importance of open communication and a support system (Feminization Center, n.d.).
Ultimately, the decision to undergo revision FFS is a deeply personal one, driven by the unwavering pursuit of an authentic self. The critical importance of selecting a highly experienced and specialized surgeon—one with a proven track record in revision procedures and a comprehensive understanding of transgender facial aesthetics—cannot be overstated. Such a surgeon not only possesses the technical skill to navigate previously altered anatomy but also the artistic vision to sculpt features that are both naturally feminine and uniquely tailored to the individual. By embracing a holistic approach that prioritizes meticulous planning, advanced techniques, and compassionate post-operative care, individuals can navigate the complexities of revision FFS with greater confidence, ultimately achieving the profound sense of harmony and self-acceptance they seek. This iterative process in facial feminization is a testament to the continuous evolution of surgical science and the unwavering human spirit in pursuit of identity congruence, transforming not just faces, but lives.
Wat is revisie-FFS?
Revision Facial Feminization Surgery (FFS) is a specialized set of procedures performed to correct or refine suboptimal aesthetic or functional outcomes from a previous FFS. It aims to further harmonize facial features with a patient’s desired feminine appearance.
Why might someone need revision FFS?
Reasons can include under-correction or over-correction of features, persistent asymmetry, visible scarring, incomplete feminization, evolving aesthetic preferences, or, rarely, complications from the initial surgery.
Hoe lang moet ik wachten voordat ik overweeg om FFS te herzien?
Most surgeons recommend waiting a minimum of 6 to 18 months after the initial surgery. This allows for complete resolution of swelling and for soft tissues to fully settle, ensuring that any perceived irregularities are stable and genuinely warrant further intervention.
Is revision FFS more complex than initial FFS?
Yes, revision FFS can be more intricate due to the presence of scar tissue, altered anatomical planes, and potentially compromised tissue integrity from prior surgery. It requires a surgeon with advanced expertise and meticulous planning.
What role does advanced imaging play in revision FFS?
Advanced 3D imaging, such as CT scans with 3D reconstruction, and virtual surgical planning (VSP) are crucial. They provide detailed insights into underlying bone structure and allow surgeons to precisely plan corrective actions, design custom guides, and simulate outcomes.
Are soft tissue revisions common in revision FFS?
Yes, soft tissue revisions are often necessary to manage scars, address residual skin laxity, or refine volume through techniques like surgical scar revision, laser treatments, thread lifts, or targeted fat grafting.
Bibliografie
- Allure Esthetic. (n.d.). Revision Facial Feminization Seattle. Opgehaald van https://www.allureesthetic.com/transgender/revision-facial-feminization/
- Dr. MFO. (2024, April 9). De ultieme FFS-revisiegids: Als dingen niet volgens plan gaan. Opgehaald van https://www.dr-mfo.com/the-ultimate-ffs-revision-guide/
- Dr. MFO. (2025, July 22). FFS-revisiechirurgie: wat u kunt verwachten na gecombineerde procedures. Opgehaald van https://www.dr-mfo.com/ffs-revision-surgery-combined-procedures/
- Facialteam. (n.d.). Redoing Facial Feminization Surgery. Opgehaald van https://facialteam.eu/redoing-facial-feminization-surgery/
- Feminization Center. (n.d.). Achieve Your Vision: A Guide to Transformative Redo FFS (Revision Facial Feminization Surgery). Opgehaald van https://feminizationcenter.com/redo-ffs-surgery/
- Centrum voor geslachtsbevestiging. (nd). Facial Feminization Surgery (FFS) & Gender-Affirming Facial Surgery 101. Opgehaald van https://www.genderconfirmation.com/what-is-ffs/
- Gursky, A. K., Chinta, S. R., Wyatt, H. P., Belisario, M. N., Shah, A. R., Kantar, R. S., & Rodriguez, E. D. (2024). A Comprehensive Analysis of Genioplasty in Facial Feminization Surgery: A Systematic Review and Institutional Cohort Study. Journal of Clinical Medicine, 14(1), 182. https://pmc.ncbi.nlm.nih.gov/articles/PMC11721636/
- Het Spiegel Centrum. (nd). De evolutie van gezichtsfeminisatiechirurgie. Opgehaald van https://www.drspiegel.com/transgender/the-evolution-of-facial-feminization-surgery/





