A tracheal shave, also known as a cricothyroidotomy, is a surgical procedure used to create a temporary airway opening in the trachea (windpipe). This procedure is typically performed in emergency situations when a patient is experiencing severe airway obstruction and conventional methods of securing an airway, such as intubation, are unsuccessful or impossible. It’s a life-saving intervention, but it’s crucial to understand the procedure, its risks, and the recovery process. This article provides a comprehensive overview of tracheal shaving to inform both medical professionals and the public.

Table of Contents
Understanding Tracheal Shaving
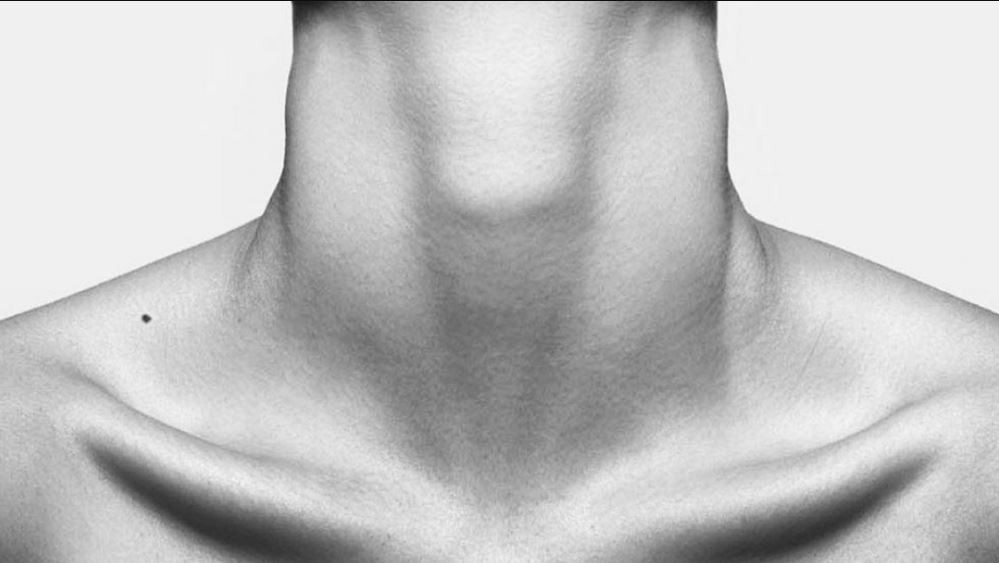
A tracheal shave is a relatively quick and straightforward procedure, particularly compared to a formal tracheostomy. It involves making a small incision through the skin and underlying tissues of the neck, directly over the cricothyroid membrane – the thin membrane located between the cricoid cartilage (the lowest ring of the trachea) and the thyroid cartilage (the Adam’s apple). This membrane is relatively avascular, meaning it has a reduced blood supply, minimizing bleeding during the procedure. The incision exposes the tracheal lumen (the airway), allowing for the immediate insertion of an endotracheal tube or tracheostomy tube to establish an airway. The term “shave” refers to the fact that the incision is typically superficial, shaving away only a small amount of tissue.
Unlike a formal tracheostomy, which involves creating a permanent opening in the trachea, a tracheal shave is intended to be a temporary measure. It’s primarily used in emergency situations where rapid airway access is critical, such as severe airway edema (swelling) from allergic reactions, trauma, or burns. It provides a quick pathway for ventilation until more definitive airway management can be established. The procedure is often performed by emergency medical personnel, anesthesiologists, or other trained medical professionals in settings where immediate airway intervention is paramount.
The decision to perform a tracheal shave is based on the urgency of the situation and the inability to secure the airway through other means. Factors influencing this decision include the severity of airway obstruction, the availability of other airway management techniques, and the skill level of the medical personnel present. It’s a procedure that requires a thorough understanding of anatomy and a precise technique to minimize complications.
The key difference between a tracheal shave and a tracheostomy lies in the depth and permanence of the incision. A tracheostomy is a more involved procedure, creating a larger opening and often involving a longer recovery period. A tracheal shave, by contrast, is a smaller, temporary solution aimed at providing immediate airway access.
The Procedure: A Step-by-Step Guide
The procedure typically begins with the patient’s neck being carefully cleaned and sterilized. Local anesthesia may be used, although in life-threatening emergencies, this step might be omitted due to time constraints. A horizontal incision is then made across the cricothyroid membrane, usually about 1-2 centimeters in length. This incision cuts through the skin, subcutaneous tissue, and the cricothyroid membrane itself. Careful dissection is crucial to avoid damaging surrounding structures, such as the thyroid gland or major blood vessels.
Once the cricothyroid membrane is exposed, a small tracheal hook or similar instrument is often used to gently spread the incision, further opening the airway. A tracheal tube, typically a smaller endotracheal tube, is then inserted directly into the trachea through the incision. This tube is connected to a ventilator or bag-valve mask to provide assisted ventilation. The tube is secured in place, and the patient’s respiratory status is closely monitored.
The precise technique may vary slightly depending on the individual patient’s anatomy and the specific circumstances. However, the core principles remain consistent: a small, precisely placed incision to rapidly access the trachea and establish an airway. The procedure’s speed and simplicity are its primary advantages in emergency settings.
Following successful insertion of the tracheal tube, the wound is often left open to allow for drainage and ventilation. In some cases, a temporary dressing may be applied to protect the site. The patient’s oxygen saturation and respiratory rate are carefully monitored post-procedure.
Risks and Potential Complications
While a tracheal shave is a life-saving procedure, it carries inherent risks and potential complications. One of the most significant risks is bleeding. Although the cricothyroid membrane is relatively avascular, significant bleeding can occur if major blood vessels are inadvertently damaged during the incision. This can compromise the airway and make ventilation difficult. Infection is another potential complication, particularly if the procedure is performed in a non-sterile environment or if proper wound care is not followed.
Damage to surrounding structures, such as the thyroid gland, vocal cords, or esophagus, is also a possibility, though relatively rare with skilled practitioners. Such damage can lead to long-term complications, including voice changes or swallowing difficulties. Subcutaneous emphysema, the accumulation of air in the tissues beneath the skin, can also occur, causing swelling and discomfort. This is typically managed conservatively.
Airway obstruction can persist even after the procedure if the incision is inadequate or if there is significant swelling or bleeding. In such cases, further intervention, such as a formal tracheostomy, may be necessary. The risk of these complications is higher if the procedure is performed by less experienced personnel or in challenging circumstances.
Proper training and adherence to sterile techniques are crucial in minimizing these risks. Careful patient selection and a thorough understanding of the anatomy are also essential to ensure a successful and safe procedure.
Recovery and Aftercare Advice
After a tracheal shave, the patient will be closely monitored for respiratory status and any signs of complications. The tracheal tube is typically left in place for a period determined by the patient’s clinical condition. Once the underlying cause of airway obstruction is resolved and the patient can breathe adequately on their own, the tube can be removed. The wound is usually left open to drain, and it will heal by secondary intention, meaning it fills in gradually from the bottom up.
Pain management is an important aspect of recovery. Pain medication is often prescribed to manage any discomfort at the incision site. Regular wound cleaning and dressing changes may be necessary to prevent infection. Patients may experience some hoarseness or voice changes temporarily due to the proximity of the incision to the vocal cords. This typically resolves as the wound heals.
Regular follow-up appointments are essential to monitor the healing process and address any concerns. Patients should be instructed on proper wound care and advised to avoid strenuous activities that could strain the incision site. The recovery time varies depending on individual factors and the patient’s overall health, but complete healing usually takes several weeks.
Patients should be educated on the signs and symptoms of infection, such as increased pain, swelling, redness, or pus at the incision site, and instructed to seek medical attention immediately if these occur. A successful recovery depends on close monitoring, proper wound care, and adherence to the physician’s instructions.
A tracheal shave is a critical life-saving procedure used in emergency situations to establish a temporary airway. While effective and relatively simple to perform, it carries potential risks and requires careful consideration. Understanding the procedure, its risks, and the recovery process is crucial for both medical professionals and patients. Successful outcomes depend on appropriate patient selection, skilled execution, and diligent post-operative care.
Visit Dr.MFO Instagram profile to see real patient transformations! Get a glimpse of the incredible results achieved through facial feminization surgery and other procedures. The profile showcases before-and-after photos that highlight Dr. MFO’s expertise and artistic vision in creating natural-looking, beautiful outcomes.
Ready to take the next step in your journey? Schedule a free consultation with Dr. MFO ( Best Facial Feminization Surgeon for You) today. During the consultation, you can discuss your goals, ask any questions you may have, and learn more about how Dr. MFO can help you achieve your desired look. Don’t hesitate to take advantage of this free opportunity to explore your options and see if Dr. MFO is the right fit for you.
https://en.wikipedia.org/wiki/Chondrolaryngoplasty









