Facial Feminization Surgery (FFS) is a complex and highly individualized set of procedures aimed at modifying facial features to create a more feminine appearance. Among the most impactful of these procedures is forehead contouring, as the forehead is a primary indicator of perceived gender due to inherent differences in the underlying bony structure. A prominent brow ridge and a forward-sloping forehead are typically considered masculine traits, while a smoother, more vertically oriented forehead is associated with femininity. Successfully addressing the forehead can dramatically alter the facial profile and contribute significantly to a harmonious and feminine aesthetic.
As a surgeon specializing in FFS, I approach forehead contouring with meticulous planning and a deep understanding of the intricate anatomy of the frontal bone and its relationship to vital underlying structures. The goal is not merely to reduce projection but to create a smooth, natural-looking contour that integrates seamlessly with the rest of the face. Achieving this requires selecting the appropriate surgical technique, primarily choosing between two distinct methods: bone shaving, also known as Type 1 contouring, and forehead osteotomy, often referred to as Type 3 contouring.
The decision between these techniques is paramount and is dictated by the patient’s unique anatomy, specifically the thickness of the frontal bone and the size and position of the frontal sinus. This discussion will delve into the intricacies of both bone shaving and osteotomy, providing a comprehensive overview from a surgeon’s viewpoint, examining the indications, techniques, advantages, disadvantages, and potential complications of each, ultimately guiding the understanding of why one method is chosen over the other for a specific patient.
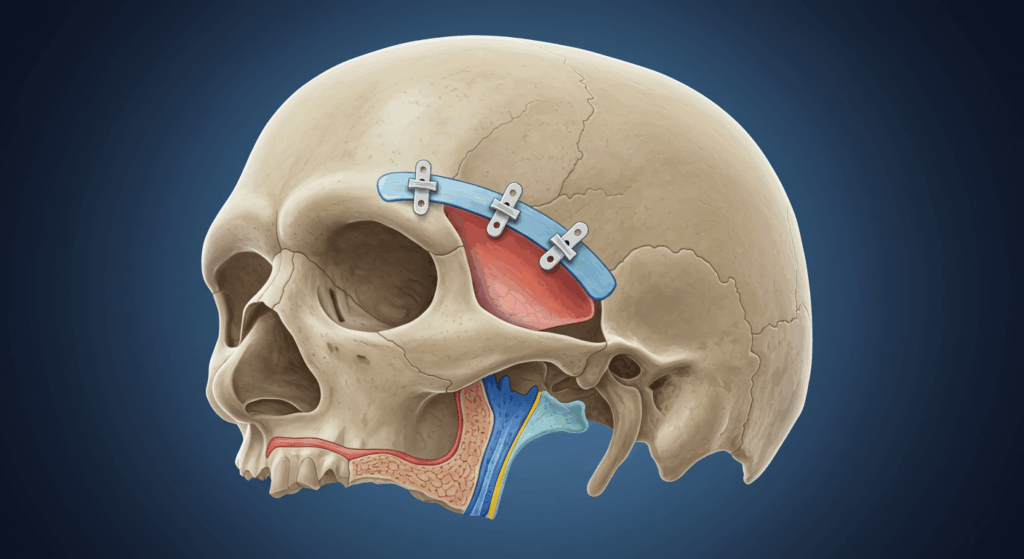
Table of Contents
Understanding the Forehead: Relevant Anatomy for Contouring
To comprehend the surgical approaches to forehead contouring, one must first appreciate the detailed anatomy of the frontal bone. The frontal bone forms the forehead and the upper part of the eye sockets (orbits). Key features relevant to FFS include:
The Glabella and Supraorbital Rims
The glabella is the smooth, triangular area on the forehead above the bridge of the nose and between the eyebrows. In individuals with masculine features, the glabella often forms part of a prominent brow ridge. The supraorbital rims are the bony arches that form the upper margins of the eye sockets. In masculine foreheads, these rims can be thicker and project further forward than in feminine foreheads. The degree of projection in both the glabella and supraorbital rims is a primary target for feminization.
Frontal Bossing
Frontal bossing refers to the prominence or forward projection of the forehead bone, particularly in the supraorbital region (above the eyes). The degree and location of this bossing vary significantly between individuals. Reducing this bossing is a core objective of forehead contouring.
The Frontal Sinus
Critically, the frontal bone contains the frontal sinuses, which are air-filled cavities located within the bone, typically situated behind the lower central part of the forehead, often extending superiorly. The size and extent of the frontal sinuses are highly variable. Understanding the position and size of the frontal sinus is essential for surgical planning, as it significantly impacts the feasibility of bone shaving and necessitates an osteotomy when the sinus is large and contributes to the frontal bossing. The anterior wall of the frontal sinus is the bone that forms the outer surface of the forehead in this region. The posterior wall separates the sinus from the intracranial contents (the brain and its coverings).
Bone Thickness and Layers
The frontal bone, like other skull bones, is composed of layers. There is an outer table (the outer layer), an inner table (the inner layer facing the brain), and a layer of spongy bone called the diploë sandwiched between them. The thickness of the frontal bone varies across the forehead and between individuals. Crucially, the thickness of the outer table, particularly over the frontal sinus, determines how much bone can be safely removed during bone shaving without entering the sinus cavity.
Important Adjacent Structures
Surrounding the frontal bone are vital structures that must be protected during surgery. These include the supraorbital and supratrochlear nerves (branches of the trigeminal nerve providing sensation to the forehead and scalp), blood vessels (supplying the scalp and forehead), and the dura mater (the tough outer membrane covering the brain), which lies immediately deep to the inner table of the skull. Damage to these structures can lead to complications such as numbness, bleeding, or even cerebrospinal fluid (CSF) leakage.
A thorough understanding of these anatomical elements, particularly the relationship between the frontal bossing, the supraorbital rims, the frontal sinus size, and the thickness of the outer table, forms the basis for selecting the appropriate surgical technique for forehead feminization. Pre-operative imaging, specifically a computed tomography (CT) scan, is indispensable for accurately mapping these structures and planning the surgical approach.
Bone Shaving: Type 1 Forehead Contouring
Bone shaving, often referred to as Type 1 forehead contouring, is the less invasive of the two primary techniques for reducing frontal bossing. This method involves carefully reducing the thickness of the frontal bone using specialized surgical instruments.
Ideal Candidates for Bone Shaving
Bone shaving is suitable for patients who exhibit minimal to moderate frontal bossing and, critically, have a thick enough frontal bone anterior to the frontal sinus. This technique is most effective when the primary cause of the forehead prominence is simply thicker bone, rather than the outward bulging caused by a large underlying frontal sinus. In cases where the frontal sinus is small or absent, bone shaving can often achieve a satisfactory level of reduction and contouring.
Patients with significant brow ridge prominence that is primarily due to thick bone above a small or recessed frontal sinus are also good candidates. A CT scan is essential to confirm that sufficient bone thickness exists over the sinus to allow for safe and effective shaving. If the outer table of the frontal bone over the sinus is thin, aggressive shaving would risk perforating the sinus cavity, which is undesirable.
The Surgical Technique of Bone Shaving
The procedure is typically performed under general anesthesia. Access to the forehead bone is most commonly gained through a coronal incision. This incision is made behind the hairline, extending from ear to ear, allowing the surgeon to lift the scalp flap forward to expose the entire forehead bone. The advantage of a coronal incision is that the resulting scar is hidden within the hair. For individuals with a receding hairline, a pre-trichial incision (made just in front of the hairline) may be considered to simultaneously lower the hairline, though this results in a visible scar at the hairline.
Once the frontal bone is exposed, the surgeon uses specialized instruments, primarily high-speed surgical burrs (essentially medical drills with various shapes and sizes of heads) and sometimes rasps, to carefully and gradually remove layers of the outer bone. The burrs allow for precise and controlled reduction of the bone thickness. The surgeon works meticulously to reduce the prominence of the glabella and supraorbital rims, aiming to create a smoother, more rounded contour.
The process involves carefully assessing the amount of bone to be removed, constantly checking the thickness of the remaining bone to avoid entering the frontal sinus or significantly thinning the bone to a point of weakness. This requires tactile feedback and a thorough understanding of the pre-operative CT scan data, which serves as a surgical roadmap indicating areas of varying bone thickness and the location of the frontal sinus. The goal is to feather the edges of the shaved area smoothly into the surrounding bone to avoid creating palpable steps or irregularities.
Advantages of Bone Shaving
From a surgical perspective, bone shaving offers several advantages when the patient’s anatomy is suitable:
- Less Invasive: Compared to osteotomy, bone shaving is a less extensive procedure. It does not involve cutting and repositioning large segments of bone or manipulating the frontal sinus cavity.
- Faster Recovery: Patients typically experience a quicker recovery period following bone shaving due to the reduced surgical trauma. Swelling and bruising may be less severe and resolve more quickly.
- Lower Risk Profile: Generally, bone shaving carries a lower risk of complications compared to osteotomy. Risks associated with bone healing, hardware, and direct manipulation of the frontal sinus are significantly reduced or eliminated.
- Shorter Operative Time: The surgical time for bone shaving is typically shorter than for a forehead osteotomy.
- No Need for Internal Fixation: Unlike osteotomy, bone shaving does not require the use of plates, screws, or wires to stabilize bone segments, avoiding potential issues related to hardware.
Limitations of Bone Shaving
Despite its advantages, bone shaving has significant limitations that make it unsuitable for many patients requiring forehead feminization:
- Limited Scope of Correction: The primary limitation is that bone shaving can only reduce the projection to the extent allowed by the thickness of the outer table of the frontal bone over the frontal sinus. If the frontal bossing is primarily due to a large, protruding frontal sinus, shaving the outer bone will not significantly reduce the overall projection without risking sinus perforation.
- Inability to Address Significant Frontal Bossing or Prominent Supraorbital Rims: When the brow ridge and forehead projection are substantial and linked to a large frontal sinus, bone shaving alone is insufficient to achieve adequate feminization. The underlying bony structure dictates the maximum achievable reduction.
- Risk of Over-Resection and Thinning: Aggressive shaving in areas of thin bone, particularly over the frontal sinus, can lead to unintentional entry into the sinus cavity. Over-thinning the bone can also weaken it, potentially making it more susceptible to fracture.
- Potential for Irregularities: While meticulous technique minimizes this risk, uneven bone removal can potentially lead to subtle contour irregularities or palpable steps under the skin.
In summary, bone shaving is an excellent technique for appropriate candidates with minimal to moderate frontal bossing and favorable bone thickness over the frontal sinus. However, it is crucial to understand its limitations and recognize when a more extensive procedure is necessary to achieve the desired aesthetic outcome. The decision hinges entirely on the pre-operative anatomical assessment, primarily through CT imaging.
Forehead Osteotomy: Type 3 Forehead Contouring
Forehead osteotomy, or Type 3 forehead contouring, is a more involved surgical procedure indicated for patients with significant frontal bossing, particularly when this prominence is caused by a large or forward-projecting frontal sinus, and/or when significant reduction of the supraorbital rims is required. This technique allows for a much greater degree of contouring and feminization compared to bone shaving.
Ideal Candidates for Forehead Osteotomy
Patients who benefit most from a forehead osteotomy are those exhibiting moderate to severe frontal bossing, often associated with a large frontal sinus that extends significantly forward. These individuals typically have a prominent brow ridge that cannot be adequately reduced by simple bone shaving without compromising the integrity of the frontal sinus wall. Forehead osteotomy is also the preferred method when substantial reshaping or reduction of the supraorbital rims is necessary to achieve a more feminine eye socket shape. The CT scan findings, specifically the size and position of the frontal sinus and the relative projection of the brow ridge, are the primary determinants of candidacy for this procedure.
The Surgical Technique of Forehead Osteotomy
Similar to bone shaving, forehead osteotomy is performed under general anesthesia, and access is typically gained through a coronal or pre-trichial incision. Once the forehead bone is exposed, the key difference lies in the approach. Instead of simply shaving the surface, the surgeon performs precise cuts (osteotomies) in the bone to remove or reposition a segment.
The most common type of forehead osteotomy for feminization involves removing the anterior wall of the frontal sinus. After carefully outlining the section of bone to be removed, using measurements and potentially a template based on pre-operative planning, the surgeon uses specialized saws (like oscillating saws) and osteotomes (bone chisels) to make cuts in the bone surrounding the frontal sinus anterior wall and extending to the supraorbital rims. The precise pattern of these cuts is planned pre-operatively based on the desired contour and the patient’s anatomy.
Once the bone segment, often encompassing the anterior wall of the frontal sinus and the supraorbital rims, is carefully removed, the underlying frontal sinus cavity is exposed. Any bony septations (internal divisions) within the sinus that contribute to the outward bulge are carefully burred away to create a smooth inner contour. The removed bone segment is then reshaped on a separate sterile field. This reshaping often involves reducing its projection, smoothing its surface, and potentially altering the shape of the supraorbital rims incorporated within the segment.
After reshaping, the bone segment is re-inserted into the forehead defect in a recessed position to reduce the overall frontal projection. The repositioned bone segment is then fixed securely in place using small titanium plates and screws. These plates and screws provide stability and allow the bone to heal in its new position. In some cases, if the bone segment is unsuitable for replacement (e.g., too thin or fragmented), the defect in the forehead may be reconstructed using bone graft material (either from another part of the skull or a synthetic substitute) or a bone cement specifically designed for cranioplasty (skull reconstruction). However, utilizing the patient’s own reshaped bone is often the preferred method when feasible.
The surgeon meticulously contours the edges of the repositioned bone segment to blend smoothly with the surrounding native bone, often using burrs to refine the final shape and ensure a seamless transition. The goal is to create a smooth, feminine curvature to the forehead.
Advantages of Forehead Osteotomy
Forehead osteotomy offers significant advantages when the patient’s anatomy necessitates a more comprehensive approach:
- Greater Degree of Correction: This is the primary advantage. Osteotomy allows for substantial reduction of severe frontal bossing and prominent supraorbital rims, achieving a level of feminization often impossible with bone shaving alone. It directly addresses the projection caused by a large frontal sinus.
- Ability to Reshape the Supraorbital Rims: Osteotomy allows for more significant manipulation and reshaping of the supraorbital rims, contributing significantly to feminizing the eye area.
- Creates a Smooth, Uniform Contour: By removing, reshaping, and repositioning a segment of bone, the surgeon can create a consistently smooth and feminine contour across the forehead, even in cases of significant pre-existing irregularities.
- Addresses the Underlying Sinus: While direct manipulation of the sinus carries risks, addressing the sinus directly by removing its anterior wall is necessary when the sinus is the primary cause of the bossing.
Disadvantages of Forehead Osteotomy
As a more invasive procedure, forehead osteotomy also comes with a higher risk profile and longer recovery:
- More Invasive: This procedure involves cutting and manipulating bone, exposing the frontal sinus cavity, and requiring internal fixation. This inherently makes it more invasive than bone shaving.
- Longer Recovery Period: Patients undergoing osteotomy typically experience more significant swelling, bruising, and discomfort, leading to a longer overall recovery time compared to bone shaving.
- Higher Risk of Complications: The risks associated with osteotomy are more numerous and potentially more serious. These include complications related to the frontal sinus (infection, mucocoele formation, CSF leak), complications related to the bone healing (non-union, malunion), complications related to the fixation hardware (infection, palpability, need for removal), contour irregularities, nerve injury, and dural tears.
- Potential for Hardware Palpability: In individuals with thin skin, the underlying plates and screws used for fixation may be palpable through the skin, although this is often not visible. Rarely, hardware may become infected or cause discomfort and require removal in a subsequent procedure.
- Risk to the Frontal Sinus: Entry into the frontal sinus cavity during surgery carries the risk of infection migrating into the sinus or even intracranially if the posterior sinus wall is compromised. Careful surgical technique and post-operative care are crucial to minimize these risks.
- Risk of CSF Leak: Although rare, there is a risk of inadvertently tearing the dura (the brain’s protective covering) during the procedure, particularly if the posterior wall of the frontal sinus is very thin or adherent to the dura. A dural tear can lead to a cerebrospinal fluid (CSF) leak, which requires prompt recognition and management to prevent serious complications like meningitis.
Despite the increased risks and longer recovery, forehead osteotomy is often the only way to achieve the desired level of feminization for patients with significant frontal bossing. The decision to proceed with an osteotomy is made after a thorough discussion of the risks and benefits with the patient, ensuring they have realistic expectations regarding the outcome and recovery.

Comparing Bone Shaving and Osteotomy: The Decision-Making Process
Choosing between bone shaving (Type 1) and forehead osteotomy (Type 3) is perhaps the most critical decision in forehead contouring and is a prime example of how individualized surgical planning is essential in FFS. This is not a one-size-fits-all scenario; the optimal technique is entirely dictated by the patient’s specific anatomy and surgical goals.
The cornerstone of this decision-making process is the pre-operative assessment, with the CT scan serving as the indispensable tool. A high-resolution CT scan provides detailed, cross-sectional images of the frontal bone, allowing the surgeon to precisely evaluate:
- The thickness of the frontal bone across the entire forehead.
- The size, shape, and extent of the frontal sinus.
- The relationship of the frontal sinus to the areas of greatest frontal bossing and supraorbital rim projection.
- The thickness of the anterior wall of the frontal sinus.
- The relationship of the inner table of the frontal bone to the underlying dura.
Based on the CT findings, the surgeon can determine whether sufficient bone thickness exists over the frontal sinus to allow for adequate reduction through shaving alone (indicating Type 1 is feasible) or if the frontal bossing is predominantly due to a large, protruding frontal sinus or requires more significant supraorbital rim reduction than shaving can provide (indicating Type 3 is necessary).
Key Factors Differentiating the Decision
Let’s summarize the key differences that guide the surgeon’s choice:
| Feature | Bone Shaving (Type 1) | Forehead Osteotomy (Type 3) |
| Indications | Minimal to moderate frontal bossing; Thick frontal bone over sinus; Small or absent frontal sinus. | Moderate to severe frontal bossing; Large/protruding frontal sinus; Need for significant supraorbital rim reduction. |
| Mechanism | Reducing bone thickness with burrs/rasps. | Cutting, removing, reshaping, and repositioning a bone segment; Addressing the frontal sinus directly. |
| Scope of Correction | Limited by bone thickness over sinus. | Allows for significant reduction and reshaping. |
| Invasiveness | Less invasive. | More invasive. |
| Recovery Time | Shorter. | Longer. |
| Risk Profile | Lower. | Higher (especially risks related to frontal sinus and bone healing). |
| Need for Hardware | No. | Yes (plates and screws for fixation). |
| Impact on Frontal Sinus | Avoided if possible; Risk of perforation if bone is thin. | Directly addressed; Risk of sinus-related complications. |
| Scar Location | Typically coronal (behind hairline) or pre-trichial (at hairline). | Typically coronal (behind hairline) or pre-trichial (at hairline). |
In a patient with mild frontal bossing and a thick frontal bone anterior to a small sinus, bone shaving may be sufficient to achieve a good result with lower risk and faster recovery. Conversely, a patient with severe frontal bossing caused by a large, forward-extending frontal sinus will necessitate an osteotomy to achieve meaningful feminization. Attempting bone shaving in such a case would be ineffective and potentially dangerous due to the high risk of entering the large sinus cavity without achieving adequate contouring.
The surgeon’s role is to integrate the anatomical findings from the CT scan with the patient’s aesthetic goals and risk tolerance. A detailed discussion with the patient about the pros and cons of each technique, based on their specific anatomy, is crucial for informed consent and setting realistic expectations. While some patients may prefer the less invasive option of bone shaving, it is the surgeon’s responsibility to explain when this technique is inadequate and that an osteotomy is necessary to achieve the desired level of feminization.
It is also important to note that there are variations and combinations of techniques, sometimes referred to as Type 2 contouring (which might involve shaving the supraorbital rim and performing an osteotomy of the anterior sinus wall), but the core distinction between simply reducing bone thickness (shaving) and cutting/repositioning bone (osteotomy) remains fundamental to the surgical approach. For the purpose of this detailed discussion focusing on the primary differences, we concentrate on the clear distinction between Type 1 (shaving) and Type 3 (osteotomy).
Ultimately, the decision is a surgical judgment based on a comprehensive anatomical assessment and a thorough understanding of the capabilities and limitations of each procedure. The aim is always to achieve the best possible aesthetic outcome while prioritizing patient safety.
Surgical Planning and Execution: Meticulous Steps for a Successful Outcome
Regardless of whether bone shaving or osteotomy is performed, meticulous surgical planning and execution are paramount to achieving a successful outcome in forehead contouring. The process begins long before the patient enters the operating room.
Pre-operative Assessment
The pre-operative phase is critical. It involves a comprehensive assessment of the patient, including:
- Medical History and Physical Examination: A thorough review of the patient’s overall health, any pre-existing medical conditions, medications, allergies, and previous surgeries. A physical examination of the face and forehead contour is performed, evaluating the degree of bossing, the shape of the supraorbital rims, and the skin and soft tissue quality.
- Psychological Evaluation: While not always mandatory, a psychological evaluation can be beneficial to ensure the patient is mentally prepared for surgery, has realistic expectations, and is undergoing surgery for appropriate reasons. FFS is a deeply personal journey, and emotional preparedness is key.
- Photography: Standardized photographs are taken from various angles to document the pre-operative appearance and serve as a reference during planning and for evaluating the post-operative result.
- Computed Tomography (CT) Scan: As previously emphasized, a high-resolution CT scan of the facial skeleton, particularly focusing on the frontal bone and sinuses, is indispensable. This allows for detailed visualization of the underlying bony anatomy, including bone thickness, sinus size and extent, and the relationship of these structures to the outer contour. Some surgeons utilize 3D reconstructive software to further analyze the CT data and plan the osteotomy cuts or areas of bone reduction.
Based on this comprehensive assessment, the surgeon formulates a detailed surgical plan, determining the specific technique (shaving or osteotomy), the extent of bone reduction or repositioning required, the planned osteotomy lines (if applicable), and strategies for managing adjacent structures.
Anesthesia
Forehead contouring procedures are typically performed under general anesthesia to ensure patient comfort and immobility throughout the surgery.
Incision Planning and Execution
The choice and execution of the incision are crucial for both access and minimizing visible scarring.
- Coronal Incision: The most common approach is the coronal incision, made within the hair-bearing scalp, extending from ear to ear across the top of the head. This provides excellent exposure of the entire frontal bone. The incision is carefully planned to avoid major blood vessels and nerves within the scalp. The skin edges are beveled to allow hair follicles to grow through the scar, making it less visible.
- Pre-trichial Incision: For patients with a high hairline who desire concomitant hairline lowering, a pre-trichial incision is made just in front of the hairline. This allows for simultaneous advancement of the scalp and hairline while providing access to the forehead bone. The scar is located at the hairline, which some patients find acceptable given the benefit of a lower hairline. Careful technique is required to create a fine-line scar that mimics the natural hairline.
After making the incision, the scalp and forehead skin are carefully dissected away from the underlying bone, creating a surgical flap that exposes the entire frontal bone down to the supraorbital rims. This dissection is carried out in a specific plane to minimize bleeding and protect vital structures.
Surgical Execution: Step-by-Step
While the specific steps differ significantly between bone shaving and osteotomy after exposure, some principles are universal:
- Hemostasis: Meticulous control of bleeding is essential throughout the procedure to maintain a clear surgical field and minimize post-operative bruising and swelling.
- Protection of Nerves: Special care is taken to identify and protect the supraorbital and supratrochlear nerves as they emerge from the supraorbital rims and course across the forehead and scalp. Damage to these nerves can result in temporary or permanent numbness in the forehead and scalp.
- Bone Reshaping/Manipulation:
- Bone Shaving: Using high-speed burrs, the surgeon carefully and incrementally removes bone from the glabella and supraorbital rims, constantly checking the thickness to avoid perforating the frontal sinus. The goal is to create a smooth, convex contour.
- Forehead Osteotomy: Following the pre-operative plan, precise osteotomy cuts are made using specialized saws. The bone segment is carefully elevated, the frontal sinus cavity is addressed (if necessary, septations are removed and the lining is inspected), the bone segment is reshaped using burrs, and then it is repositioned in a more recessed position. Small titanium plates and screws are used to rigidly fix the bone in its new location.
- Contouring and Smoothing: After the primary reduction or repositioning, the surgeon meticulously smooths the transitions between the treated area and the surrounding bone using burrs, ensuring a natural-looking contour without palpable steps or irregularities.
- Irrigation: The surgical field is thoroughly irrigated with sterile saline solution to remove bone dust and debris, which helps prevent infection.
- Closure: Once the bone work is complete, the scalp flap is carefully redraped. Drainage tubes may be placed temporarily to collect any excess fluid or blood. The incision is closed in layers using sutures or surgical staples. The closure is performed meticulously to minimize scarring and ensure proper wound healing.
Post-operative Considerations in the Operating Room
Before the patient is woken up, dressings are applied. A compressive dressing may be used initially to help reduce swelling and bruising. The patient is then transferred to the recovery room for close monitoring as they emerge from anesthesia.
The successful execution of either bone shaving or osteotomy requires not only technical skill but also a deep understanding of surgical anatomy, meticulous planning, and the ability to adapt the plan based on intra-operative findings. The surgeon’s experience in performing FFS procedures, particularly forehead contouring, is a significant factor in achieving optimal results and minimizing complications.
Post-operative Care and Recovery: Navigating the Healing Process
The post-operative period is a crucial phase in forehead contouring recovery. The specific timeline and challenges vary depending on whether bone shaving or osteotomy was performed, with osteotomy generally requiring a longer and more intensive recovery.
Immediate Post-operative Period
Immediately after surgery, patients will experience swelling, bruising, and discomfort in the forehead and scalp. Pain medication will be administered to manage discomfort. A head dressing is often applied to provide gentle compression and reduce swelling. Drainage tubes, if placed, will remain in place for a day or two to collect any post-operative fluid or blood.
Patients undergoing bone shaving may be able to go home the same day or stay one night in the hospital. For osteotomy, a hospital stay of one to several nights is more common to monitor for potential complications such as excessive bleeding, swelling, or issues related to the frontal sinus.
Managing Swelling and Bruising
Swelling and bruising are universal after forehead contouring and can be quite noticeable. Swelling typically peaks within the first 48-72 hours and then gradually subsides over the following weeks. Bruising may initially appear around the eyes and can spread down the face before resolving. Strategies to manage swelling and bruising include:
- Head Elevation: Keeping the head elevated, even while sleeping, helps reduce swelling by promoting fluid drainage.
- Cold Compresses: Applying cold compresses to the forehead and surrounding areas (avoiding direct pressure on the incision) can help constrict blood vessels and minimize swelling and bruising in the initial days.
- Medications: Anti-inflammatory medications (prescribed by the surgeon) can help reduce swelling.
The resolution of swelling and bruising takes time, and patients should be prepared for their appearance to look different from the final result for several weeks or even months. Significant swelling may persist for 3-4 weeks, with residual subtle swelling taking several more months to fully resolve.
Pain Management
Discomfort is expected after surgery. Pain medication will be prescribed to manage this. The level of pain varies, but osteotomy generally involves more post-operative pain due to the more extensive bone manipulation. Most patients can transition from prescription pain medication to over-the-counter pain relievers within a week or two.
Incision Care
Proper care of the incision is essential for good wound healing and minimizing scarring. The surgeon will provide specific instructions on how to clean the incision and whether any ointments should be applied. Sutures or staples are typically removed 1-2 weeks after surgery. Itching along the incision line is common as it heals.
Numbness and Paresthesia
Numbness in the forehead and scalp is a very common experience after both bone shaving and osteotomy due to temporary disruption or stretching of the small nerves that supply sensation to the area. Patients may also experience paresthesia, which is a tingling or “pins and needles” sensation, as the nerves begin to regenerate. While sensation typically returns gradually over several months, some degree of permanent numbness in certain areas is possible, particularly along the incision line. For osteotomy, numbness in the forehead below the incision is expected due to the flap elevation. Sensation typically returns, but it can take many months.
Activity Restrictions
Patients will need to restrict their activities during the initial recovery period. Strenuous activity, heavy lifting, and activities that increase blood pressure should be avoided for several weeks to minimize swelling and reduce the risk of bleeding or wound complications. The surgeon will provide specific guidelines on when it is safe to resume normal activities, exercise, and work.
Recovery Timeline
The recovery timeline differs between bone shaving and osteotomy:
- Bone Shaving: Patients can often return to light, non-strenuous work within 1-2 weeks. More strenuous activities can usually be resumed within 4-6 weeks. While initial swelling subsides relatively quickly, subtle swelling may linger for a few months.
- Forehead Osteotomy: Recovery is generally longer. Patients may require 2-4 weeks off work, depending on the nature of their job. Strenuous activities are typically restricted for 6-8 weeks. Significant swelling and bruising take longer to resolve, and it may take several months for the final contour to become apparent as the bone heals and swelling completely dissipates.
Long-term Recovery and Final Results
The final results of forehead contouring become increasingly apparent as swelling resolves and the bone heals. For osteotomy, complete bone healing can take several months. The forehead contour will continue to refine over this period. The long-term outcome is a smoother, more feminine forehead contour that harmonizes with the rest of the facial features. Regular follow-up appointments with the surgeon are necessary to monitor healing, address any concerns, and evaluate the final result.
It is crucial for patients to be patient during the recovery process and understand that the final aesthetic outcome will not be immediately visible. Swelling and bruising can be discouraging, but they are temporary. Following the surgeon’s post-operative instructions diligently is essential for optimal healing and minimizing complications.
Potential Risks and Complications: Understanding the Possibilities
Like any surgical procedure, forehead contouring, whether bone shaving or osteotomy, carries potential risks and complications. While serious complications are rare in the hands of an experienced FFS surgeon, patients must be aware of the possibilities. The risk profile is generally higher for osteotomy due to its greater invasiveness and involvement of the frontal sinus.
General Surgical Risks
These risks are common to most surgical procedures and are not specific to forehead contouring:
- Infection: Infection is a risk whenever an incision is made. Signs of infection include increased pain, redness, swelling, warmth, and pus drainage. Infections require prompt medical attention and antibiotic treatment. In severe cases, surgical drainage may be necessary.
- Bleeding (Hematoma): Excessive bleeding under the skin can lead to a hematoma (a collection of blood). A small hematoma may resolve on its own, but a larger one may require surgical drainage.
- Seroma: A seroma is a collection of clear fluid under the skin. Like hematomas, small seromas may resolve spontaneously, while larger ones may require aspiration (drawing out the fluid with a needle).
- Anesthesia Complications: Risks associated with general anesthesia include adverse reactions to medications, respiratory problems, or cardiovascular events. These risks are minimized by a thorough pre-operative medical evaluation and the presence of an experienced anesthesiologist.
- Poor Wound Healing: Factors such as smoking, poor nutrition, or underlying medical conditions can impair wound healing, potentially leading to delayed healing, wound separation, or wider scars.
Procedure-Specific Risks for Bone Shaving (Type 1)
While generally lower risk than osteotomy, bone shaving has its own specific potential complications:
- Over-Resection: Shaving too much bone can lead to an overly flattened or concave area, or, more seriously, perforate the anterior wall of the frontal sinus.
- Bone Irregularities: Uneven bone removal can result in palpable steps or irregularities under the skin. While minor irregularities may not be visible, significant ones can be aesthetically displeasing and potentially require revision surgery.
- Nerve Injury: As mentioned in the anatomy section, the supraorbital and supratrochlear nerves are at risk during the dissection and bone work. Injury can lead to temporary or permanent numbness or altered sensation in the forehead and scalp.
- Insufficient Correction: If the frontal bossing is more significant than initially assessed or the bone over the sinus is thinner than anticipated, bone shaving may not achieve the desired level of feminization, potentially requiring a secondary procedure (possibly an osteotomy).
Procedure-Specific Risks for Forehead Osteotomy (Type 3)
Osteotomy carries a higher risk profile primarily due to the manipulation of the bone, exposure of the frontal sinus, and the use of hardware:
- Frontal Sinus Complications: This is a significant area of concern. Risks include:
- Sinus Infection: Infection within the frontal sinus can occur if bacteria are introduced during surgery or if the sinus is not properly managed. A sinus infection can be painful and, in rare cases, can spread to surrounding structures.
- Mucocoele: A mucocoele is a cyst-like swelling filled with mucus that can form if the frontal sinus drainage pathway is blocked after surgery. Mucocoeles can enlarge over time, causing pain and pressure, and may require surgical drainage or removal.
- CSF Leak: Although rare, a dural tear during the procedure can result in a leak of cerebrospinal fluid (CSF). A CSF leak is a serious complication that can lead to meningitis (infection of the membranes surrounding the brain and spinal cord). Signs include a clear, watery nasal discharge (if the leak is into the nose via the sinus) or persistent headache. Prompt diagnosis and management, which may involve surgical repair of the dural tear, are essential.
- Hardware Complications:
- Infection: The titanium plates and screws used for fixation can become infected, requiring antibiotic treatment or, in some cases, surgical removal of the hardware.
- Palpability: In individuals with thin skin, the hardware may be palpable under the skin. While usually not visible, it can be a source of discomfort for some patients, and removal can be considered after bone healing is complete (typically after 6-12 months).
- Migration or Loosening: Although rare with modern fixation techniques, the plates and screws could potentially loosen or migrate, requiring revision surgery.
- Bone Healing Complications:
- Non-union: In rare cases, the repositioned bone segment may fail to heal properly, resulting in a “non-union.” This may require further surgery to promote bone healing.
- Malunion: The bone segment may heal in an undesirable position, leading to contour irregularities.
- Contour Irregularities: Despite careful planning and execution, subtle contour irregularities can occur after osteotomy, potentially requiring minor revision procedures to refine the shape.
- Nerve Injury: Similar to bone shaving, the supraorbital and supratrochlear nerves are at risk. Additionally, branches of the facial nerve that control forehead movement are also at risk, although temporary weakness or asymmetry is more common than permanent paralysis.
- Persistent Pain: Chronic pain in the forehead region is a rare but possible complication after osteotomy.
- Undesirable Aesthetic Outcome: While the goal is feminization, there is always a risk that the aesthetic outcome may not fully meet the patient’s expectations, even if the surgery is technically successful. This highlights the importance of realistic expectations and clear communication with the surgeon during the planning phase.
Discussing these potential risks and complications in detail with the patient during the consultation process is crucial for informed consent. While this list may seem extensive, the actual incidence of serious complications is low in experienced hands. The surgeon takes numerous precautions to minimize these risks during every step of the procedure.
Patient Selection and Expectations: Ensuring a Good Fit
Selecting the appropriate candidates for forehead contouring and managing patient expectations are as important as the surgical technique itself. Not every individual seeking forehead feminization is an ideal candidate for surgery, and ensuring a good match between the patient’s goals and what surgery can realistically achieve is vital for patient satisfaction.
Ideal Candidates
Ideal candidates for forehead contouring in FFS, whether for bone shaving or osteotomy, typically share several characteristics:
- Good Physical Health: Patients should be in good overall health to tolerate surgery and anesthesia. Underlying medical conditions that could increase surgical risks should be well-controlled or appropriately managed.
- Non-Smoker: Smoking significantly impairs wound healing and increases the risk of complications. Surgeons often require patients to stop smoking well in advance of surgery.
- Realistic Expectations: Patients should have a clear and realistic understanding of what forehead contouring can achieve and its limitations. They should understand that the goal is feminization, not necessarily achieving a perfect or completely different appearance.
- Psychological Preparedness: Patients should be emotionally stable and undergoing surgery for their own personal reasons and well-being, not due to external pressure. A positive self-image and acceptance of the recovery process contribute to greater satisfaction.
- Anatomical Suitability: As discussed extensively, the underlying bony anatomy, particularly the frontal bossing and frontal sinus, must be suitable for the chosen technique to achieve a significant and safe result.
Setting Realistic Expectations
It is the surgeon’s responsibility to thoroughly discuss the anticipated outcome of forehead contouring with the patient, based on their specific anatomy. This involves:
- Reviewing CT Scans: Showing the patient their CT scans and explaining how their anatomy dictates the surgical approach and the degree of possible reduction.
- Discussing the Chosen Technique: Clearly explaining why bone shaving or osteotomy is recommended for them, detailing the procedure, and highlighting the expected results and limitations of that specific technique.
- Visual Aids: Utilizing pre-operative photographs and potentially 3D imaging or morphing software (with the caveat that morphing is a simulation and not a guarantee of the outcome) to help the patient visualize the potential post-operative changes.
- Discussing the Recovery Process: Providing a realistic overview of the recovery timeline, expected swelling, bruising, discomfort, and activity restrictions.
- Reviewing Potential Risks and Complications: Ensuring the patient fully understands the potential risks associated with the chosen procedure.
Patients should understand that while forehead contouring can dramatically improve the forehead profile, it may not completely eliminate all signs of previous masculine features, nor can it change the underlying bone structure beyond what is surgically feasible and safe. Minor asymmetries or subtle irregularities may persist. The goal is a significant improvement towards a more feminine contour that is in harmony with the rest of their feminized facial features.
The Importance of Choosing an Experienced FFS Surgeon
Forehead contouring, particularly osteotomy, is a technically demanding procedure that requires specialized knowledge of facial anatomy and extensive experience in craniofacial and aesthetic surgery. Choosing a surgeon with significant experience in performing FFS procedures, specifically forehead contouring, is paramount for optimizing results and minimizing complications. An experienced surgeon will be able to accurately assess the patient’s anatomy, choose the appropriate technique, execute the surgery meticulously, and manage potential complications effectively. Patients should research their surgeon’s credentials, experience, and view before-and-after photos of their previous patients to gain confidence in their abilities.
Effective patient selection and clear, honest communication regarding expectations are foundational to achieving high levels of patient satisfaction in forehead contouring.
Long-term Outcomes and Follow-up: The Journey Continues
The journey of forehead contouring does not end when the patient leaves the operating room or even after the initial recovery period. The long-term outcomes and scheduled follow-up appointments are important aspects of the process.
Evolution of Results Over Time
While the initial reduction in forehead projection is apparent immediately after surgery (though masked by swelling), the final contour continues to refine over several months as swelling completely resolves and, in the case of osteotomy, as the bone heals and remodels. Subtle changes in contour and soft tissue settling will occur. Patients should be patient and allow sufficient time for the full results to become apparent.
Potential Need for Revision Surgery
While the vast majority of patients are satisfied with the results of their primary forehead contouring surgery performed by an experienced surgeon, there is a small possibility that revision surgery may be considered in some cases. Reasons for revision could include:
- Insufficient Correction: If the initial reduction was not as significant as desired or anticipated.
- Contour Irregularities: If there are palpable steps, depressions, or asymmetries that are aesthetically bothersome.
- Hardware Issues (after Osteotomy): If hardware becomes infected, palpable, or causes discomfort after bone healing.
- Complications: Addressing complications like a persistent mucocoele or a delayed bone healing issue.
Revision surgery for forehead contouring is often more complex than the primary procedure due to altered anatomy and scar tissue. The need for revision is relatively low, but it is a possibility that patients should be aware of. A thorough discussion between the patient and surgeon is necessary to determine if revision is warranted and what could realistically be achieved.
Scheduled Follow-up Appointments
Regular follow-up appointments with the surgeon are essential throughout the recovery process and beyond. These appointments allow the surgeon to:
- Monitor wound healing and incision sites.
- Assess the resolution of swelling and bruising.
- Evaluate the healing of the bone (after osteotomy).
- Address any patient concerns or questions.
- Monitor for any signs of complications.
- Assess the aesthetic outcome and discuss further steps if necessary.
Initial follow-up appointments are typically scheduled frequently in the weeks immediately following surgery. As healing progresses, the frequency of appointments decreases. Long-term follow-up, sometimes years after surgery, can also be beneficial to ensure the stability of the result and address any late-onset issues.
Stability of the Outcome
Once the bone has healed and the soft tissues have settled, the results of forehead contouring are generally considered stable and permanent. The reshaped or repositioned bone forms the new, feminine forehead contour. While the natural aging process will continue to affect the skin and soft tissues over time, the underlying bony structure is permanently altered.
The long-term success of forehead contouring is a testament to the meticulous planning and execution of the surgical procedure and the patient’s diligent adherence to post-operative care instructions.
Conclusion: Choosing the Path to a Feminine Forehead
Forehead contouring is a powerful and transformative component of Facial Feminization Surgery, significantly impacting the perceived gender of an individual. The choice between bone shaving (Type 1) and forehead osteotomy (Type 3) is a critical surgical decision, guided not by preference alone, but by the intricate and unique anatomy of each patient’s frontal bone and the overlying frontal sinus.
Bone shaving, the less invasive technique, is suitable for individuals with mild to moderate frontal bossing and sufficient bone thickness anterior to a small or absent frontal sinus. It offers a quicker recovery and a lower risk profile. However, its limitations lie in its inability to address significant frontal bossing caused by a large frontal sinus or to achieve substantial reshaping of prominent supraorbital rims.
Forehead osteotomy, while more invasive, is the necessary technique for patients with moderate to severe frontal bossing, particularly when a large frontal sinus dictates the outward projection. It allows for significant bone reduction and reshaping, offering a greater degree of feminization and the ability to effectively address prominent supraorbital rims. However, this increased capability comes with a longer recovery period and a higher risk profile, including potential complications related to the frontal sinus and bone healing.
The surgeon’s expertise in interpreting pre-operative imaging, specifically the CT scan, is paramount in determining the most appropriate technique for each individual patient. This anatomical assessment, combined with a thorough understanding of the patient’s aesthetic goals and risk tolerance, forms the basis of the individualized surgical plan.
Forehead contouring, regardless of the technique employed, requires meticulous surgical execution, careful attention to anatomical details, and diligent post-operative care. While potential risks and complications exist for both procedures, they are minimized in the hands of an experienced FFS surgeon.
Ultimately, the goal of forehead contouring is to create a smooth, harmonious, and feminine forehead contour that enhances the overall facial aesthetic and contributes to the patient’s journey of self-affirmation. By understanding the fundamental differences between bone shaving and osteotomy, the indications for each, and the associated risks and recoveries, both surgeons and patients can make informed decisions that lead to the safest and most aesthetically pleasing outcomes in forehead feminization. The journey to a feminine forehead is a collaborative effort between a skilled surgeon and a well-informed patient, working together to achieve transformative results.
Visit Dr.MFO Instagram profile to see real patient transformations! Get a glimpse of the incredible results achieved through facial feminization surgery and other procedures. The profile showcases before-and-after photos that highlight Dr. MFO’s expertise and artistic vision in creating natural-looking, beautiful outcomes.
Ready to take the next step in your journey? Schedule a free consultation with Dr. MFO ( Best Facial Feminization Surgeon for You) today. During the consultation, you can discuss your goals, ask any questions you may have, and learn more about how Dr. MFO can help you achieve your desired look. Don’t hesitate to take advantage of this free opportunity to explore your options and see if Dr. MFO is the right fit for you.










