The journey of gender affirmation often involves significant physical transformations to align an individual’s outward appearance with their internal gender identity. For many, facial features play a crucial role in gender perception, making facial gender-affirming surgeries (FGAS), such as Facial Feminization Surgery (FFS) and Facial Masculinization Surgery (FMS), pivotal. This guide delves into the cutting-edge use of 3D printing technology to create custom facial implants and surgical guides, revolutionizing FGAS by offering personalized solutions for enhanced facial harmony. While the term “bioprinting” often implies printing with biological materials or living cells, in the context of custom facial implants for FGAS, 3D printing refers to advanced additive manufacturing techniques used to produce patient-specific, biocompatible implants and tools that integrate seamlessly with natural tissues, thereby enhancing the precision and outcomes of these transformative procedures.
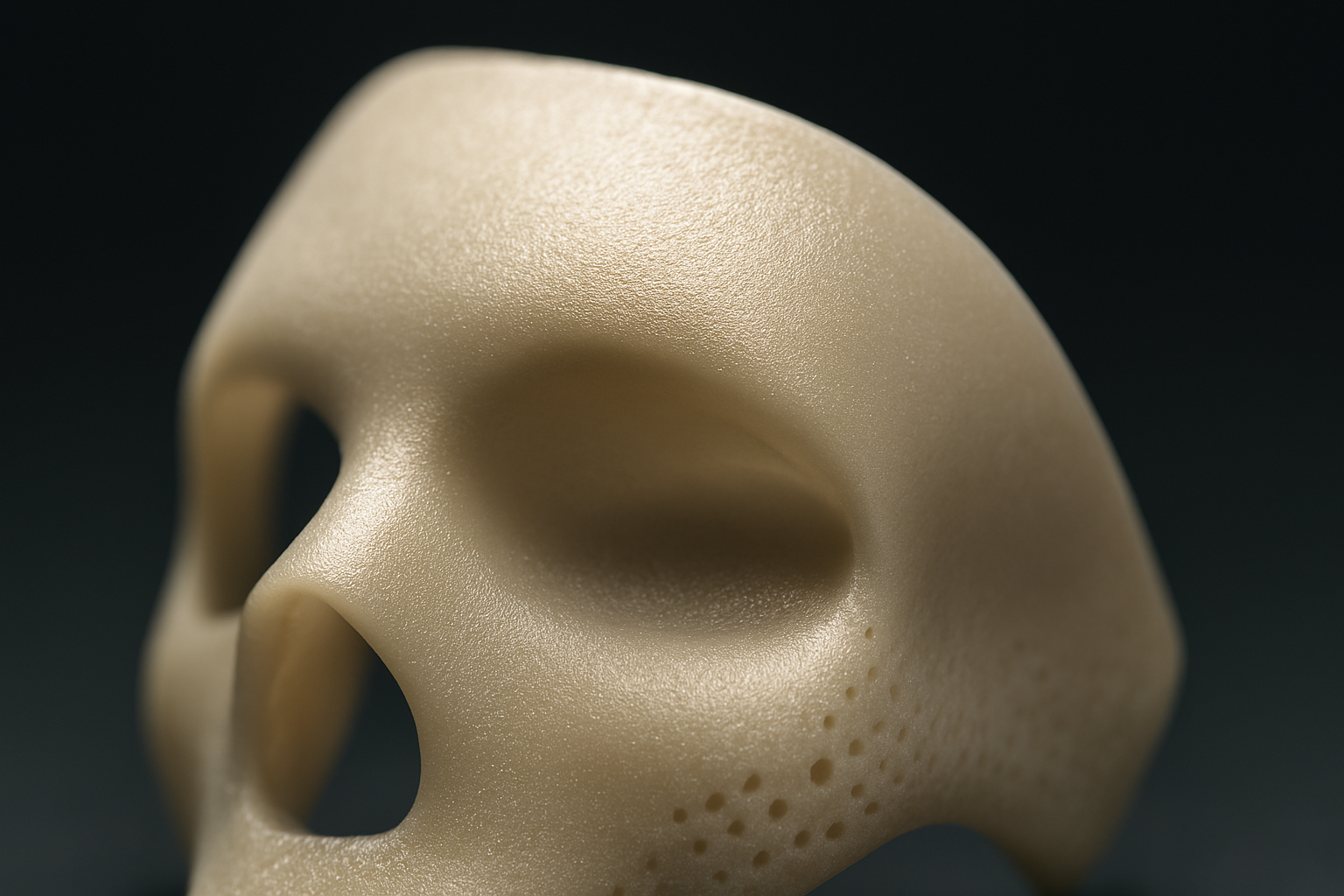
Table of Contents
Understanding 3D Printing in Medical Applications
Overview of 3D Printing: How it Works and Its Applications in Modern Medicine
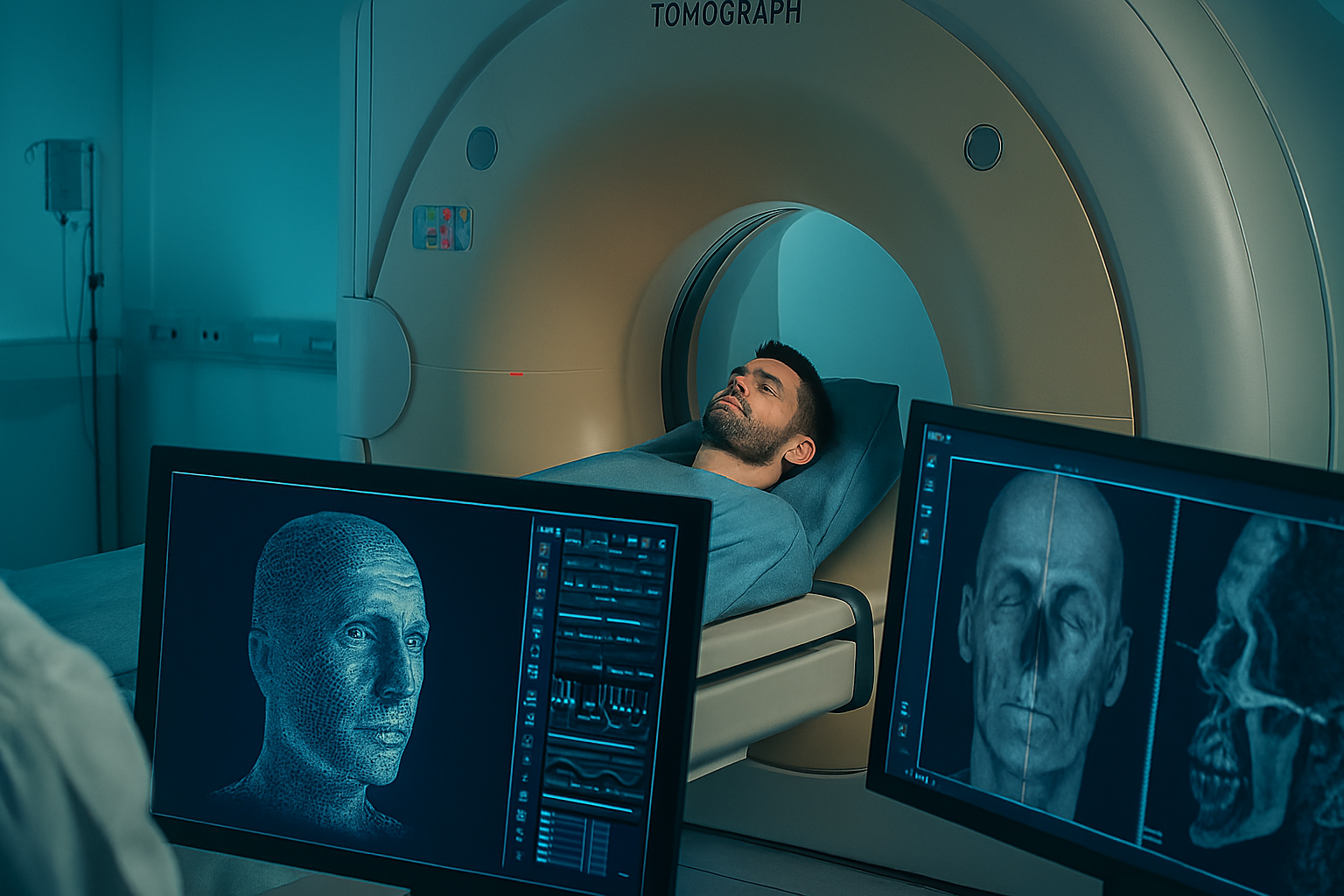
3D printing, or additive manufacturing, involves building three-dimensional objects layer by layer from a digital design. In modern medicine, this technology has numerous applications, from creating anatomical models for surgical planning to producing custom prosthetics and implants. For facial gender-affirming surgeries, a key application is Virtual Surgical Planning (VSP) and the creation of 3D-printed guides and patient-specific models (Sharaf et al., 2022). This process typically begins with image acquisition, most commonly a maxillofacial computed tomography (CT) scan. The data from the CT scan is then segmented, which involves extracting regions of interest and outlining anatomical structures. This segmented data is then exported into a 3D Standard Tessellation Language (.STL) file (Sharaf et al., 2022).
The Advantages of 3D Printing Over Traditional Implant Manufacturing Techniques
The advantages of 3D printing, particularly in the context of VSP, over traditional methods are significant. These technologies improve the safety, accuracy, and efficiency of facial feminization surgeries (Sharaf et al., 2022). Traditionally, surgeons might rely on their experience and intraoperative assessments, which, while skilled, cannot match the precision offered by a pre-planned, digitally guided approach. 3D printing allows for the creation of patient-specific models and cutting guides, which can be used to delineate frontal sinus boundaries, plan mandibular angle reductions, and guide osseous genioplasties with enhanced precision (Sharaf et al., 2022).
How Biocompatible Materials Ensure Safety and Integration with Natural Tissues
While the provided sources don’t delve into the specifics of “bioprinted” implants in terms of living tissue, they highlight the fabrication of “custom plates” that can be pre-bent on 3D models and sterilized for use during procedures like osseous genioplasty (Sharaf et al., 2022). The emphasis on safety, accuracy, and reduced complications with 3D printed guides and planned osteotomies inherently points to the use of biocompatible materials for any implanted components. The goal is to ensure these patient-specific solutions integrate safely and effectively with the patient’s natural tissues, minimizing risks such as infection or rejection (Sharaf et al., 2022).
The Need for Custom Facial Implants in Gender-Affirming Surgeries
Challenges in Achieving Precise, Individualized Results with Conventional Implants
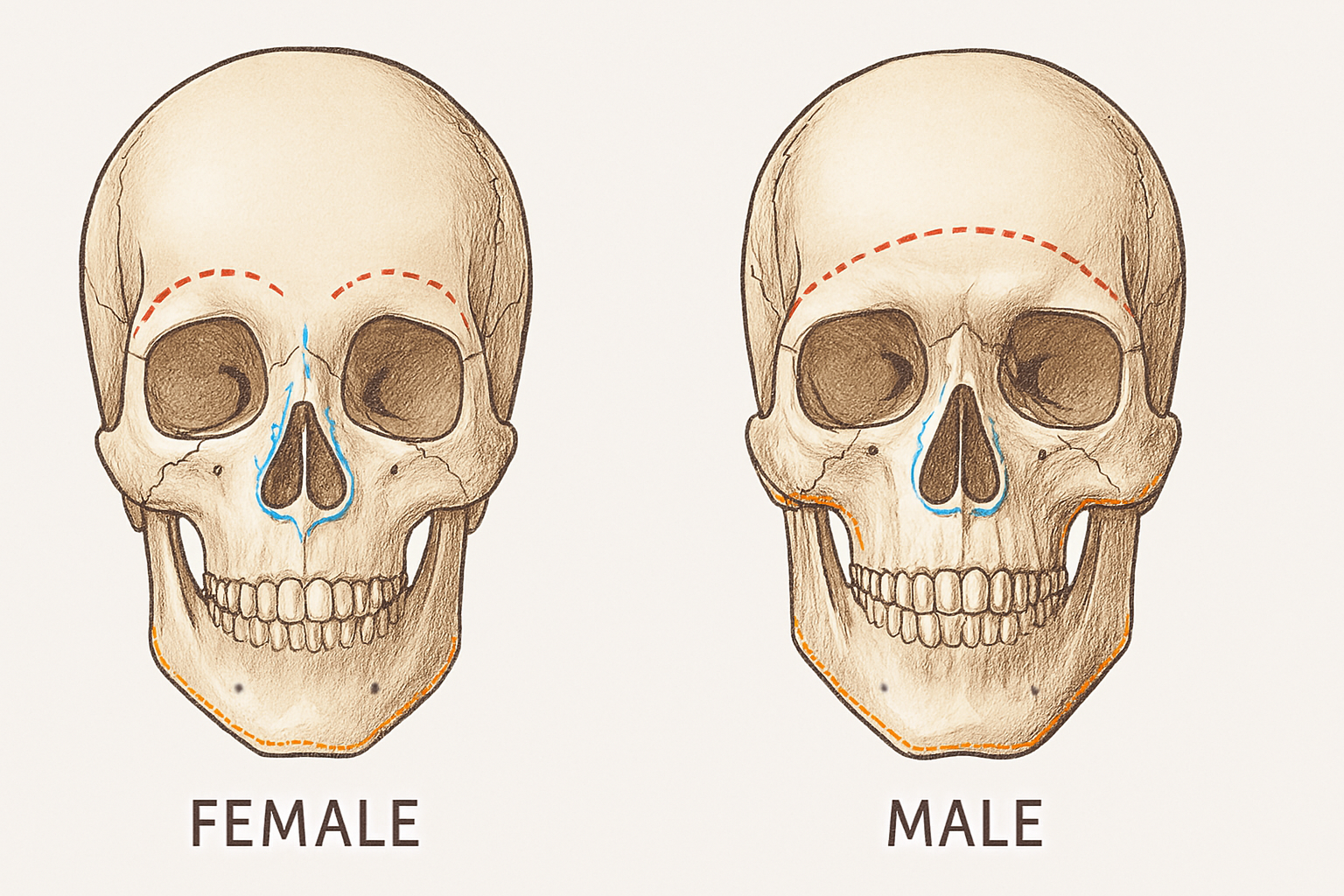
Gender-affirming facial surgery aims to create facial features that better reflect an individual’s gender identity. Until recently, there were few objective guidelines to justify and facilitate effective surgical decision-making for these complex procedures (Seth et al., 2022). The human face exhibits significant differences between sexes, with male faces typically being larger (7.3% on average) and showing distinct shape variations in areas like the brow, jaw, nose, and cheek (Seth et al., 2022). Conventional implants, often pre-manufactured in standard sizes and shapes, struggle to address these unique, individualized anatomical differences. This can lead to less precise results and a diminished sense of facial harmony.
How Custom Implants Address Unique Anatomical Differences in FFS and FMS
Custom implants, designed using advanced 3D printing and VSP, directly tackle the limitations of conventional approaches. For FFS, for example, the masculine mandible is wider, has thicker bone, and a more angular structure compared to the feminine mandible, which is more trapezoidal, shorter in height, and less angular. Similarly, the male forehead often presents with increased supraorbital bossing, a larger frontal sinus, and flatter, lower-set brows (Sharaf et al., 2022). Custom implants, along with 3D-printed cutting guides, allow surgeons to precisely address these specific anatomical nuances. This personalization ensures that alterations to the forehead, jawline, and chin are tailored to the individual’s unique facial structure, leading to a more natural and gender-affirming outcome (Sharaf et al., 2022).
The Psychological and Aesthetic Benefits of Tailored Facial Enhancements
The face plays a significant role in gender recognition and self-perception (Sharaf et al., 2022). Therefore, altering facial features to align with one’s gender identity can profoundly improve body image satisfaction and overall quality of life (Sharaf et al., 2022). Custom implants, by providing a superior fit and more harmonious results, contribute significantly to reducing gender dysphoria and improving self-perception. Studies have shown that facial feminization surgeries can lead to improved quality of life and sustained patient satisfaction (Morrison et al., as cited in Sharaf et al., 2022). The enhanced precision offered by custom 3D-printed solutions ensures that the aesthetic goals of the patient are met with greater accuracy, leading to a more profound and positive psychological impact.
How 3D Printing Enhances Facial Gender-Affirming Surgeries
The Process of Creating Custom Facial Implants Using 3D Printing Technology
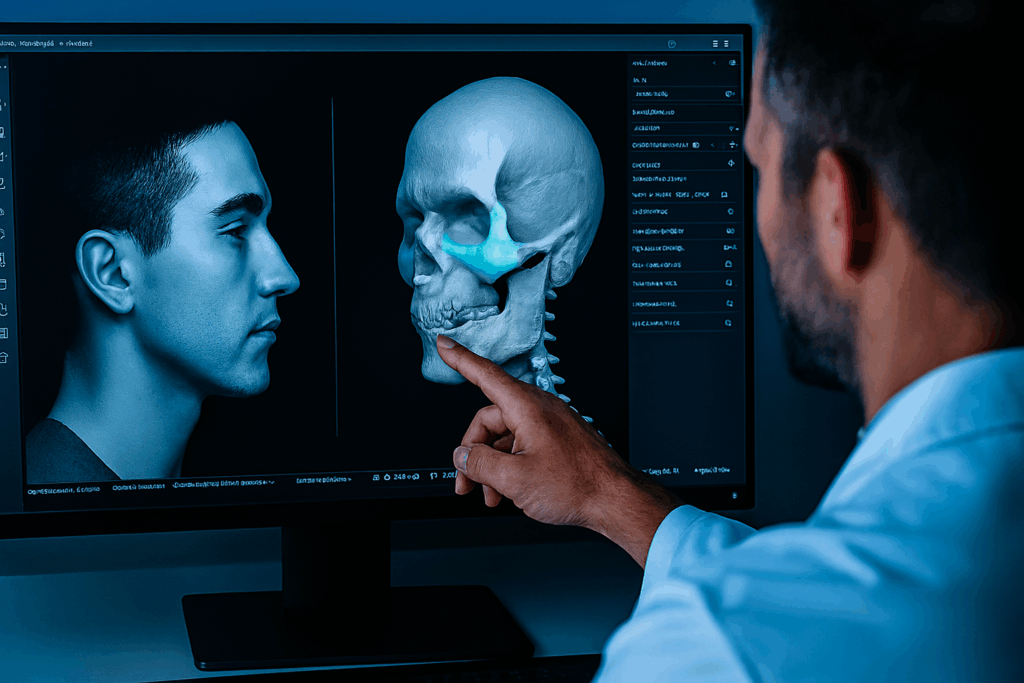
The creation of custom facial implants and surgical guides using 3D printing technology involves a meticulous process known as Virtual Surgical Planning (VSP). This process begins with acquiring high-resolution imaging, typically a maxillofacial computed tomography (CT) scan. The images are then segmented to delineate anatomical structures and areas of interest. This data is converted into a 3D Standard Tessellation Language (.STL) file. Subsequently, surgeons and biomedical engineers collaborate, often virtually, to design the surgical plan and the specific 3D models and surgical guides using specialized software like ProPlan CMF or Surgicase. Once the VSP is finalized, the surgical guides and potentially custom plates are fabricated using 3D printing (Sharaf et al., 2022).
Case Studies Showcasing the Use of 3D-Printed Implants in FFS and FMS Procedures
While specific case studies detailing the use of “bioprinted implants” in the sense of living tissue were not extensively detailed in the provided sources, the literature highlights the significant role of 3D printing in creating custom surgical guides and patient-specific models for FFS. For instance, in frontonasal-orbital contouring, 3D-printed cutting guides are used to accurately execute virtual plans for bone reduction or setback, minimizing risks like intracranial entry and improving precision. Similarly, for mandibular angle reduction and osseous genioplasty, 3D-printed models and cutting guides help surgeons plan osteotomies near critical nerves like the inferior alveolar nerve, enhancing safety and accuracy. Custom plates can also be fabricated or pre-bent on 3D models for fixation during genioplasty (Sharaf et al., 2022). These applications demonstrate how 3D printing facilitates patient-specific solutions for complex facial remodeling in gender-affirming surgeries.
The Role of Advanced Imaging Techniques in Designing Implants That Match Patients’ Facial Structures
Advanced imaging techniques, particularly maxillofacial CT, are foundational to designing implants that perfectly match a patient’s facial structure. These scans provide the detailed anatomical data necessary for the VSP process. By capturing the unique contours and bone thickness of an individual’s face, a precise digital blueprint can be created. This blueprint then guides the design of custom implants, cutting guides, and even patient-specific colored bony thickness measurement maps. These maps allow for safer execution of the surgical plan, enabling precise burring or osteotomy of the frontal bone during feminizing foreheadplasty, for example, by highlighting areas of varying bone thickness (Sharaf et al., 2022). This integration of advanced imaging and 3D design ensures that every custom component is tailored to the patient’s exact needs, leading to more natural and harmonious results.

Benefits of 3D-Printed Implants in FFS and FMS
Improved Precision and Fit, Leading to More Natural and Harmonious Results
One of the primary advantages of utilizing 3D printing in gender-affirming facial surgeries is the significant improvement in precision and fit. By leveraging Virtual Surgical Planning (VSP) and 3D-printed patient-specific guides and models, surgeons can achieve a higher level of accuracy during complex procedures (Sharaf et al., 2022). This translates to more precise alterations of bony structures, such as the forehead, jaw, and chin, ensuring that the new contours are not only aesthetically pleasing but also harmoniously integrated with the patient’s overall facial anatomy. The ability to plan and rehearse surgeries on 3D models before entering the operating room further refines this precision, leading to results that appear more natural and less “operated on” (Sharaf et al., 2022).
Reduced Risk of Complications Such as Implant Rejection or Infection
While facial feminization surgeries inherently carry risks such as infection, nerve injuries, and bony resorption, the application of VSP and 3D printing can significantly mitigate these complications (Sharaf et al., 2022). The enhanced precision in planning and execution, facilitated by patient-specific cutting guides and detailed anatomical mapping, allows surgeons to avoid critical structures like nerves and to perform osteotomies with greater control. For instance, VSP has been shown to result in safer frontal sinus wall setback procedures with less intracranial entry and safer mandibular angle reductions with less inferior alveolar nerve injury (Gray et al., as cited in Sharaf et al., 2022). Although the provided sources do not specifically discuss implant rejection in the context of “bioprinted” implants, the general improvement in surgical accuracy and safety due to 3D printing contributes to better outcomes and a reduced likelihood of various complications associated with facial surgery.
Faster Recovery Times and Enhanced Patient Satisfaction with Personalized Solutions
The increased efficiency and accuracy afforded by 3D printing in VSP can lead to reduced operative times (Gray et al., as cited in Sharaf et al., 2022). Shorter surgical durations can potentially contribute to faster initial recovery, although comprehensive facial surgery still requires significant healing time. More importantly, the ability to achieve highly personalized and predictable outcomes through custom 3D-printed solutions directly impacts patient satisfaction. Patients who undergo FFS with VSP and 3D printing have reported high satisfaction rates (Tawa et al., as cited in Sharaf et al., 2022). This is because they can review virtual plans and 3D-printed models preoperatively, allowing for a deeper understanding of the planned procedures and contributing to more realistic expectations and a greater sense of control over their transformative journey (Sharaf et al., 2022). This improved communication and shared understanding contribute significantly to enhanced patient satisfaction.
The Process of Receiving 3D-Printed Facial Implants
Step-by-Step Guide: From Initial Consultation and Imaging to Implant Design and Placement
- Initial Consultation: The journey begins with a thorough discussion between the patient and surgeon to understand the patient’s goals and concerns regarding their facial appearance. Standardized facial photographs and a comprehensive assessment of both skeletal and soft tissue units are performed (Sharaf et al., 2022).
- Advanced Imaging: A maxillofacial computed tomography (CT) scan is acquired. This is a crucial step to evaluate the intricate facial bone and sinus anatomy (Sharaf et al., 2022).
- Virtual Surgical Planning (VSP): The CT images are used to create a 3D digital model of the patient’s face. Biomedical engineers and radiologists collaborate with the surgeon to segment the images, outlining anatomical structures and areas of interest. Specialized software (e.g., ProPlan CMF, Surgicase) is used to meticulously plan the surgical procedures, including the precise extent of bone reduction or augmentation (Sharaf et al., 2022).
- 3D Printing of Models and Guides: Based on the virtual plan, sterilizable cutting guides, patient-specific models, and potentially custom plates are 3D-printed in-house or by a specialized facility. These physical models allow for pre-operative practice and help both the surgeon and patient visualize the planned outcome (Sharaf et al., 2022).
- Pre-operative Review: The patient reviews the virtual plan and 3D-printed models with the surgical team. This is a vital step for patient education, ensuring they understand the proposed surgical approaches, their anatomy, and to confirm the final surgical plan (Sharaf et al., 2022).
- Surgical Procedure and Implant Placement: During surgery, the 3D-printed cutting guides and models are utilized to execute the precisely planned osteotomies and contouring. This ensures the custom implants (or bone modifications) are placed with the highest possible accuracy and safety (Sharaf et al., 2022).
What Patients Can Expect During the 3D Printing Process and Surgical Procedure
Patients can expect a highly collaborative and transparent process. After initial imaging, they may participate in virtual or in-person meetings with the surgical team to finalize the VSP. The use of 3D-printed models before surgery can be very helpful for patients to understand the different surgical approaches and their anatomy, assisting in decision-making (Sharaf et al., 2022). During the surgical procedure, the use of 3D-printed guides translates the meticulous planning directly into the operating room, aiming for a safe, accurate, and efficient intervention (Sharaf et al., 2022).
Post-Operative Care and Follow-up to Ensure Optimal Healing and Integration
Post-operative care is crucial for optimal healing and integration of any facial modifications or implants. While the provided sources focus on the pre-operative and intra-operative phases of 3D printing, general post-operative care for FFS includes managing swelling, pain, and monitoring for complications such as infection or nerve issues (Sharaf et al., 2022). Regular follow-up appointments with the surgical team are essential to track healing progress, address any concerns, and ensure the long-term success and aesthetic integration of the surgical outcomes. The improved accuracy achieved through 3D printing in VSP is expected to contribute to a smoother recovery and better long-term results.

Real-Life Success Stories and Expert Insights
Testimonials from Patients Who Have Undergone Gender-Affirming Surgeries with 3D-Printed Implants
While the provided sources do not include direct patient testimonials, they emphasize the high satisfaction rates reported by patients who have undergone facial feminization surgery with the aid of Virtual Surgical Planning and 3D printing. For example, a prospective study by Tawa et al. (as cited in Sharaf et al., 2022) reported high patient satisfaction at 6 months’ follow-up after various FFS procedures utilizing VSP and 3D printing. The ability of these technologies to deliver precise and predictable results, closely matching the pre-surgical plan, is a key factor in achieving patient satisfaction (Sharaf et al., 2022).
Before-and-After Comparisons Highlighting the Transformative Effects of Custom Implants
The transformative effects of custom implants and precise surgical planning are evident in the significant facial changes observed in gender-affirming surgeries. While explicit “before-and-after” image comparisons were not provided in the text of the curl outputs, the research highlights how 3D facial analysis reveals distinct biological differences between male and female faces in areas like the brow, jaw, nose, and cheek (Seth et al., 2022). The objective of VSP and 3D printing is to address these differences with high accuracy, enabling surgeons to achieve the desired feminization or masculinization of facial features. The precision afforded by these tools ensures that the planned aesthetic changes are realized effectively, leading to visible and impactful transformations that align with the patient’s gender identity (Sharaf et al., 2022).
Insights from Surgeons and Biomedical Engineers on the Future of 3D Printing in Facial Surgeries
Experts in the field underscore the groundbreaking potential of 3D printing and VSP. Rahul Seth, MD, a senior author of the UCSF study, states that their data provides surgeons, patients, and insurance payers with a “life-like and surgically-oriented analysis of 3D facial size and shape to guide patients and surgeons in performing these complex and life-altering surgeries” (Seth et al., 2022). The integration of point-of-care VSP and 3D printing significantly shortens the planning process, facilitates efficient communication between the surgical team, eliminates shipping times for external services, and provides valuable educational opportunities for patients, families, and surgical trainees (Sharaf etal., 2022). The ability to perform mock surgeries on 3D-printed models before the actual procedure further enhances precision and safety. The future direction points towards broader adoption of these technologies to continue improving the safety, accuracy, and overall outcomes of facial gender-affirming surgeries (Sharaf et al., 2022).
Challenges and Future Directions in 3D Printing for Gender-Affirming Surgeries
Current Limitations, Such as Cost, Accessibility, and Technological Constraints
While 3D printing and Virtual Surgical Planning (VSP) offer significant advancements in gender-affirming facial surgeries, certain limitations currently exist. The cost associated with specialized imaging (e.g., maxillofacial CT), VSP software, 3D printing equipment, and the expertise of biomedical engineers can be substantial. Accessibility can also be a challenge, as not all surgical centers may have in-house point-of-care 3D printing capabilities, requiring reliance on external third-party companies, which can add to shipping time and communication complexities (Sharaf et al., 2022). Technological constraints, though rapidly evolving, may still present limitations in terms of the range of materials that can be printed for direct implantation and the ability to perfectly replicate the natural intricacies of biological tissues. While “custom plates” can be fabricated, the full scope of “bioprinted implants” (implying living cells) is still under development and not explicitly detailed in the provided sources for current widespread use in this context.
Ethical Considerations in the Use of 3D Printing for Personalized Medical Treatments
The ethical considerations surrounding personalized medical treatments, including those involving 3D printing for gender-affirming surgeries, are paramount. These include ensuring equitable access to advanced technologies, managing patient expectations regarding customizable outcomes, and addressing data privacy with sensitive patient anatomical information. As 3D printing allows for highly individualized modifications, it’s crucial to maintain a patient-centered approach that respects autonomy and provides comprehensive counseling about the benefits, risks, and limitations of these technologies. The discussion around potential long-term outcomes, material biocompatibility, and the ongoing need for rigorous research to validate new applications are also essential ethical considerations (Sharaf et al., 2022).
Future Advancements and the Potential for Broader Applications in Gender-Affirming Care
The future of 3D printing in gender-affirming care is bright, with continuous advancements expected to overcome current limitations. Researchers continue to refine materials for implants, aiming for even greater biocompatibility and integration. The increasing sophistication of imaging techniques and VSP software will lead to even more precise and nuanced surgical planning. As the technology becomes more accessible and cost-effective, its broader application beyond surgical guides and custom plates to a wider array of personalized implants is highly anticipated. This includes potential for more complex bone and cartilage structures, and perhaps, in the distant future, truly “bioprinted” tissue scaffolds. The goal is to further enhance the safety, accuracy, and aesthetic outcomes of facial gender-affirming surgeries, offering even more precise and satisfying transformations for individuals on their gender-affirming journey (Sharaf et al., 2022).
Conclusion
The groundbreaking potential of 3D printing in creating custom facial implants and surgical guides is profoundly impacting gender-affirming surgeries. By providing unprecedented precision, safety, and personalization, this technology is revolutionizing how individuals can achieve facial harmony that truly reflects their gender identity. From detailed virtual surgical planning to the fabrication of patient-specific guides and custom plates, 3D printing ensures a tailored approach to complex facial remodeling, addressing unique anatomical differences with remarkable accuracy. This leads to more natural-looking results, reduced risks, and significantly enhanced patient satisfaction.
As this innovative technology continues to evolve, overcoming current limitations in cost and accessibility, its role in gender-affirming care is poised for even broader applications. Individuals exploring facial gender-affirming surgeries are encouraged to discuss the integration of 3D printing and virtual surgical planning with their medical teams. Embracing these advancements can pave the way for more precise, personalized, and ultimately, more satisfying outcomes in their transformative journey towards an authentic self.
Bibliography
- Sharaf, B., Kuruoglu, D., Bite, U., & Morris, J. M. (2022). Point of Care Virtual Surgical Planning and 3D Printing in Facial Feminization Surgery. Seminars in Plastic Surgery, 36(3), 164–168. https://pmc.ncbi.nlm.nih.gov/articles/PMC9729058/
- Seth, R., Bannister, J., Juszczak, H. M., Knott, P. D., Aponte, J. D., Katz, D. C., Hallgrimsson, B., Weinberg, S., & Forkert, N. D. (2022, April 18). 3D Facial Analysis Shows Biologic Basis for Gender-Affirming Surgery. UCSF MedConnection. https://medconnection.ucsfhealth.org/news/3d-facial-analysis-shows-biologic-basis-for-gender-affirming-surgery