Facial Feminization Surgery (FFS) represents a profound and life-altering journey for individuals seeking to align their outward appearance with their authentic gender identity. It is a highly specialized field of reconstructive surgery that demands not only artistic vision but also an intricate understanding of facial anatomy and surgical precision. While FFS is widely recognized for its transformative potential, leading to significant improvements in self-perception, social integration, and overall quality of life, it is imperative to acknowledge that, like any complex medical intervention, it carries inherent risks and potential for complications.
The decision to undergo FFS is deeply personal, often marking the culmination of extensive emotional, psychological, and physical preparation. It signifies a substantial investment in one’s well-being, underscoring the critical need for a comprehensive understanding of all aspects involved, including the rare but significant challenges that may arise. This advanced discourse is not intended to diminish the overwhelmingly positive outcomes associated with FFS, but rather to serve as an authoritative resource for expert audiences on the critical importance of surgical expertise, meticulous planning, and sophisticated intervention strategies in addressing and managing complex FFS complications.
For transgender individuals, FFS is often more than a cosmetic enhancement; it is a medically necessary component of gender-affirming care, directly impacting the alleviation of gender dysphoria. Therefore, navigating potential complications—ranging from general surgical concerns to FFS-specific anatomical challenges, prolonged post-operative realities, and psychological considerations—requires a nuanced, evidence-based approach. This article delves into the advanced surgical methodologies and comprehensive management protocols employed to mitigate and resolve intricate FFS complications, ensuring long-term patient well-being and satisfaction. By exploring the mechanisms of these challenges and the sophisticated solutions available, we aim to reinforce the critical role of specialized surgical knowledge and integrated care pathways in achieving optimal, lasting results in facial feminization.
The focus here is on empowering both patients and healthcare professionals with the in-depth knowledge necessary to anticipate, diagnose, and effectively manage the most intricate scenarios in FFS. From addressing nerve regeneration complexities to resolving bone healing anomalies and refining aesthetic outcomes, a proactive and expert-driven approach is paramount. This foundational understanding allows for more informed decision-making, setting realistic expectations, and fostering resilience throughout the entire transformative process. The following sections will dissect specific types of complications, advanced diagnostic approaches, the indispensable role of specialist surgeons, and realistic outlooks for revision interventions, providing a definitive framework for navigating the most challenging aspects of facial feminization surgery.
Understanding the physiological responses to FFS is fundamental in distinguishing expected recovery phenomena from actual complications. Immediately post-surgery, the body initiates a multi-step healing process. The initial inflammatory phase, characterized by redness, swelling, warmth, and mild pain, is a natural biological response aimed at forming a clot and protecting the surgical area. This is followed by the proliferative phase, where fibroblasts produce collagen to rebuild and strengthen damaged tissues, leading to new blood vessel formation. During this stage, the surgical site may appear reddish as scar tissue begins to form, and patients might experience gradual improvements in movement as tissues regain strength. The final maturative phase, extending over several months to up to two years, involves the remodeling of scar tissue, which gradually becomes less prominent and strengthens, with temporary collagen replaced by more resilient forms. This nuanced understanding helps frame expectations and guides early identification of deviations from normal healing, allowing for timely intervention (Facialteam, 2024).
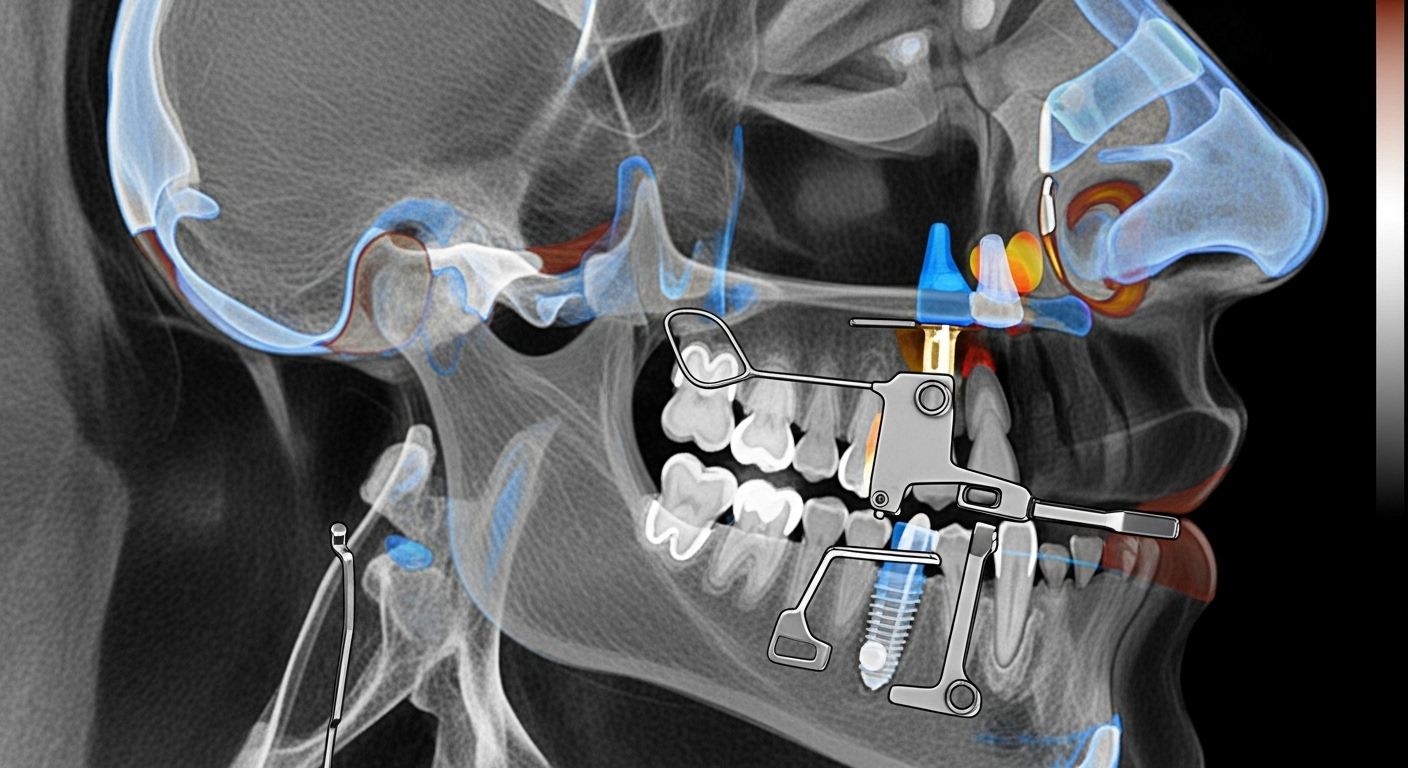
Table of Contents
Understanding Specific Complications and Advanced Interventions
Complex facial feminization surgery, while generally safe, can present unique challenges requiring advanced surgical interventions. A detailed understanding of these specific complications is crucial for effective management and optimal patient outcomes. This section delves into the nuances of various intricate issues that can arise and the sophisticated approaches employed to address them.
Nerve-Related Issues: Diagnosis and Microsurgical Repair
The intricate network of nerves in the face is highly susceptible to manipulation during FFS, leading to potential sensory or motor deficits. Sensory nerves, such as the supraorbital, supratrochlear, infraorbital, and mental nerves (branches of the trigeminal nerve), are frequently affected during forehead contouring, cheek augmentation, and chin/jaw reshaping. Post-operative numbness, tingling, or “electric shock” sensations are common as nerves regenerate, typically resolving over weeks to 18 months. However, significant or persistent numbness may indicate more extensive damage. Motor nerves, particularly branches of the facial nerve (Cranial Nerve VII), control facial expressions. Damage to these during procedures like hairline advancement, brow lift, or jaw contouring, though rare, can cause temporary or permanent weakness or paralysis, manifesting as eyebrow asymmetry or impaired smiling (Dr. MFO, 2025).
Advanced surgical interventions for nerve damage include nerve grafting, where a segment of a less critical nerve (e.g., sural nerve from the leg) is used to bridge a gap in the damaged facial nerve. Neurolysis, the surgical freeing of a nerve from scar tissue or compression, can alleviate symptoms and promote regeneration. Microsurgical repair techniques, utilizing specialized instruments and magnification, are employed for direct nerve repair, meticulously reconnecting severed nerve ends to restore function. The success of these interventions hinges on early diagnosis and the expertise of the surgical team. The great auricular nerve, responsible for sensation to the earlobe, can also be affected during jawline or neck procedures, leading to localized numbness (Facialteam, 2024).
Persistent Edema and Seroma: Advanced Drainage and Compression Strategies
While some post-operative swelling (edema) and bruising are expected after FFS, persistent or chronic fluid accumulation can impede healing and delay final aesthetic results. Swelling typically peaks within the first 1-2 weeks and largely subsides within 3-6 weeks, but residual edema, especially in areas of extensive bone work, can last 6-18 months or longer (Dr. MFO, 2025). A seroma, a collection of clear fluid, can also form under the skin. Unlike hematomas, which contain blood, seromas are usually clear or yellowish fluid and can persist if not managed.
Surgical drainage techniques are employed when seromas are large or persistent. This may involve aspiration with a needle and syringe or, in some cases, placement of a temporary surgical drain to continuously remove fluid. Specialized compression garments are vital, applying consistent pressure to reduce swelling and prevent fluid accumulation. For chronic fluid accumulation or lymphedema, which results from temporary disruption of delicate lymphatic vessels, manual lymphatic drainage (MLD) performed by a trained therapist can significantly stimulate lymphatic flow, reduce puffiness, and accelerate healing (Dr. MFO, 2025). Maintaining head elevation, applying cold compresses initially, and restricting sodium intake also contribute to managing edema.
Hardware-Related Complications: Addressing Fixation Issues
Many FFS procedures involve reshaping or repositioning facial bones, often requiring the use of fixation hardware such as plates and screws to stabilize bone segments. While generally well-tolerated, these can lead to complications. Hardware-related issues include infection, extrusion (where hardware pushes through the skin), or palpable hardware that causes discomfort or an undesirable aesthetic contour. The risk of serious complications from hardware is minimal (Gender Confirmation Center, n.d.).
Management of these complications often necessitates the removal or replacement of the hardware in a secondary surgical procedure. If an infection is present, the hardware must typically be removed, and the infection treated with antibiotics and debridement before considering replacement. In cases of palpable hardware without infection, removal can alleviate discomfort and improve aesthetic results. Careful pre-operative planning, precise placement, and selection of biocompatible materials are crucial to minimize these issues (Dr. MFO, 2025).
Bone Healing Complications: Non-Union and Malunion Correction
Procedures involving osteotomies, such as forehead setback or jaw contouring, carry a rare risk of bone healing complications. Non-union occurs when bone segments fail to fuse properly, while malunion refers to healing in an incorrect position. These can lead to persistent pain, functional deficits, or noticeable asymmetry, affecting both the structural integrity and aesthetic outcome. Reabsorption of the anterior wall of the frontal sinus, often due to improper bone cuts or weak fixation, is another specific bone healing complication that can cause functional and aesthetic problems (Facialteam, 2024).
Corrective surgical strategies for non-union or malunion typically involve re-osteotomy, where the bone is recut and repositioned, often with enhanced fixation techniques. Bone grafts, either autologous (from the patient’s own body) or allogeneic (from a donor), may be used to promote healing and fill any bone defects. Advanced imaging, such as CBCT scans, is vital for precise pre-operative planning, enabling the surgeon to identify the exact nature of the healing anomaly and devise an individualized corrective plan. Revision surgeries for bone issues require significant expertise due to altered anatomy and scar tissue (Dr. MFO, 2025).
Infection Beyond Initial Antibiotics: Surgical Debridement and Reconstruction
While the risk of infection after FFS is low with proper hygiene protocols and prophylactic antibiotics, severe or persistent infections can occur. A study on multiprocedural FFS indicated that 6 out of 31 patients experienced post-operative infection, with 4 requiring a washout procedure (Hazkour et al., 2022). Factors like preoperative dental checks, intraoperative antibiotic irrigation, and postoperative antibiotics are crucial preventative measures (Hazkour et al., 2022).
When infections do not respond to initial antibiotic therapy, surgical debridement becomes necessary. This involves the meticulous removal of infected or necrotic tissue to eliminate bacteria and promote healing. In cases involving implants or hardware, removal of the foreign body may be required to clear the infection. Following infection resolution, reconstruction may be needed to address any tissue loss or contour deformities. This can involve local tissue flaps, skin grafts, or fat grafting to restore form and function. Severe infections in jaw/chin areas can stem from dental issues due to the proximity to teeth, requiring a multidisciplinary approach involving oral and maxillofacial surgeons (Facialteam, 2024; Dr. MFO, 2025).
Unsatisfactory Aesthetic Outcomes: Advanced Revision Techniques
Achieving a harmonious and natural feminine appearance is the primary goal of FFS. However, occasionally, aesthetic outcomes may not meet patient expectations, necessitating advanced revision surgery. These issues can include significant asymmetry, contour irregularities, or functional deficits not resolved by primary surgery. Minor asymmetries are natural and often resolve with swelling, but pronounced or persistent differences may require intervention (Facialteam, 2024).
Specific surgical techniques for complex aesthetic revisions are highly personalized. Re-osteotomy may be performed to correct residual brow bossing, uneven jawline, or chin discrepancies. Fat grafting is a valuable technique for addressing severe depressions, contour deficiencies, or hollowing, using the patient’s own fat cells to add subtle volume and improve overall facial harmony. Specialized soft tissue adjustments, such as targeted excisions or repositioning of facial musculature, can correct puckering, dimpling, or unevenness in the skin overlying reshaped bone. For scarring issues, silicone-based treatments, steroid injections, laser therapy, or scar revision surgery can improve texture and color (Dr. MFO, 2025). Dissatisfaction can also stem from unmet expectations or persistent dysphoria, highlighting the importance of thorough pre-operative counseling and psychological support (Dr. MFO, 2025).
Other Specific Complications
Beyond the primary categories, other complications can arise. In forehead feminization, risks include hematoma, suture dehiscence (wound pulling apart), temporary alopecia (hair loss), and sinus issues such as perforation of the posterior wall of the frontal sinus leading to cerebrospinal fluid (CSF) leakage. CSF leaks are rare but serious, requiring immediate sealing to prevent meningitis. Sinus dysfunction, like blocked frontonasal ducts, can cause pressure or infection. Reabsorption of the anterior wall of the frontal sinus is a later complication impacting both function and aesthetics (Facialteam, 2024; Dr. MFO, 2025).
Hairline lowering, though less common, can result in poor scarring at the hairline, which can be challenging to manage due to its visibility. Jaw and chin reduction procedures carry risks such as hematoma in the floor of the mouth, which requires immediate attention to prevent airway blockage. Infections in this region can arise from dental issues. Fractures of fragile jaw areas can occur during or after surgery, necessitating immediate realignment and fixation. Tracheal shave procedures, while common, have rare risks of vocal cord damage, potentially leading to voice issues, or airway impairment from over-burring the cricothyroid membrane. Damage to salivary glands or ducts, though very rare, can result in swelling, pain, infection (sialadenitis), or a salivary fistula (Facialteam, 2024; Dr. MFO, 2025).
Diagnostic Tools and Pre-Surgical Planning for Revisions
The successful management of FFS complications, particularly in revision scenarios, hinges on meticulous diagnostic evaluation and comprehensive pre-surgical planning. This phase is paramount in identifying the precise root cause of the complication, assessing the altered anatomy, and formulating a tailored surgical strategy. Standard two-dimensional imaging provides limited insight into complex bone and soft tissue relationships, making advanced three-dimensional technologies indispensable.
Cone Beam Computed Tomography (CBCT) is a cornerstone diagnostic tool, offering high-resolution volumetric images of facial bone structures with lower radiation exposure compared to traditional CT scans. CBCT allows for detailed visualization of bone irregularities, malunion, non-union, or issues related to previously placed hardware. It can precisely pinpoint areas of inadequate bone reduction, persistent masculine contours, or even the subtle reabsorption of bone segments that might be causing aesthetic or functional concerns. This level of detail is critical for planning precise corrective osteotomies or bone grafting procedures (Dr. MFO, 2025).
Beyond static imaging, advanced 3D planning software plays a transformative role. These platforms enable surgeons to create virtual surgical simulations, allowing for a precise “rehearsal” of the revision procedure. Surgeons can virtually reposition bone segments, design custom implants for contour augmentation, or plan intricate nerve repairs. This technology facilitates accurate measurements, predicts post-operative outcomes, and minimizes surprises during the actual surgery. For example, in cases of complex asymmetry, 3D planning can highlight discrepancies that are imperceptible in standard clinical examination, guiding symmetrical re-contouring of the forehead, jaw, or chin. It also aids in identifying the optimal placement for new hardware or the removal of problematic existing hardware with minimal collateral damage.
Pre-surgical planning for revisions often extends to soft tissue analysis. While 3D bone models are crucial, understanding the overlying soft tissue envelope, scar tissue formation, and vascularity is equally important. Advanced photographic analysis, sometimes coupled with AI-driven simulations, helps to visualize potential aesthetic outcomes and manage patient expectations. In cases of nerve injury, specialized electrodiagnostic studies, such as electromyography (EMG) and nerve conduction studies (NCS), can assess the extent of nerve damage and monitor regeneration progress, informing the decision for surgical intervention versus conservative management (Dr. MFO, 2025).
Furthermore, an exhaustive review of the patient’s initial surgical records, including operative notes and previous imaging, is indispensable. This historical context provides vital information about the original procedures performed, the techniques used, and any documented intraoperative findings. For patients who underwent multiprocedural FFS, a preoperative dental check is also a key preventative measure, as issues in the oral cavity can contribute to infection risks, particularly in jaw and chin surgeries (Hazkour et al., 2022). This multi-faceted diagnostic and planning approach ensures that revision surgery is performed with the highest degree of precision, safety, and predictability, enhancing the likelihood of a successful and satisfying outcome for the patient.

The Role of the Specialist FFS Surgeon in Complication Management
The management of complex FFS complications demands a level of expertise that extends far beyond that of a general plastic surgeon. It requires a specialist FFS surgeon with an unparalleled depth of knowledge in craniofacial surgery, a nuanced understanding of gender-affirming aesthetics, and extensive experience in revision procedures. This specialization is critical for accurately diagnosing the underlying issues, formulating effective corrective strategies, and executing intricate surgical interventions.
A specialist FFS surgeon possesses an intimate understanding of the unique anatomical variations between typically masculine and feminine facial structures, and how these are altered during feminization. This knowledge is paramount when addressing complications such as persistent masculine features, disproportionate feminization, or significant asymmetries. They are adept at differentiating between expected post-operative healing phenomena and genuine complications that require intervention. For instance, distinguishing between normal post-operative swelling and lymphedema, or between temporary nerve stunning and permanent nerve damage, requires significant clinical acumen gained through dedicated experience in FFS.
Their expertise in advanced surgical techniques is equally vital. Revision FFS often involves operating in scarred tissue, which presents anatomical distortions and increased technical challenges. A specialist surgeon is proficient in intricate procedures such as re-osteotomies in previously operated bone, complex nerve repairs using microsurgical techniques, and sophisticated soft tissue rearrangements. They understand how to safely navigate altered vascular and neural pathways, minimizing further risk during corrective surgery. Furthermore, their experience allows them to judiciously apply techniques like fat grafting for contour restoration or custom implant design for precise augmentation, ensuring a harmonious and natural aesthetic outcome (Dr. MFO, 2025).
Moreover, the specialist FFS surgeon plays a crucial role in preventative measures. Through meticulous pre-operative assessment, they identify patient-specific risk factors, optimize overall health, and engage in thorough planning using 3D imaging and virtual simulations. During the initial surgery, they employ pioneering surgical techniques and stringent health protocols, including meticulous bleeding control, appropriate drain placement, and prophylactic antibiotic regimens, to minimize the incidence of complications. For example, implementing intraoperative antibiotic irrigation and locking sutures has been shown to reduce post-operative infections in multiprocedural FFS (Hazkour et al., 2022).
Beyond technical skill, a specialist FFS surgeon embodies a patient-centered approach. They engage in transparent communication, setting realistic expectations for both primary and revision surgeries. They offer comprehensive post-operative care, including structured follow-up appointments, guidance on managing recovery symptoms, and access to a supportive team that includes nurses and psychological support. Their commitment extends to addressing patient concerns promptly and empathetically, recognizing the profound emotional impact of complications. This holistic approach, combining surgical mastery with compassionate care, is fundamental to achieving both physical restoration and psychological well-being for patients navigating complex FFS challenges (Facialteam, 2024; Dr. MFO, 2025).
Patient Expectations and Realistic Outcomes for Revision
Embarking on the journey of FFS revision surgery requires a deeply informed perspective on patient expectations and the realistic outcomes that can be achieved. While primary FFS is a transformative process, revision surgery, necessitated by complications or aesthetic dissatisfaction, adds layers of complexity and emotional consideration. It is paramount for patients to engage in candid discussions with their specialist surgeon to establish clear, achievable goals and navigate the psychological landscape of corrective procedures.
Realistic expectations for revision surgery differ significantly from those for primary procedures. The presence of scar tissue from previous operations alters the facial anatomy, affects tissue elasticity, and can make dissection more challenging. This means that while significant improvements are often possible, achieving “perfection” or a flawless outcome may not always be surgically feasible. Patients should understand that the goal of revision is to ameliorate specific concerns, correct deficiencies, and enhance overall harmony rather than to achieve an idealized image that might defy anatomical limitations or the realities of prior surgical alterations (Dr. MFO, 2025).
For individuals seeking revision for persistent asymmetry, contour irregularities, or palpable hardware, the outcomes can be highly satisfying, especially when performed by an experienced revision surgeon. Specialists in FFS revisions possess the refined skills to address these specific issues through targeted bone contouring, soft tissue adjustments, or the precise removal of problematic implants (Dr. MFO, 2025). However, the healing process for revisions can be protracted, with swelling and bruising potentially lasting longer due to disrupted lymphatic pathways and increased tissue manipulation. Scar maturation, too, will follow its own timeline, often requiring patience and diligent scar care over many months (Dr. MFO, 2025).
Psychological adjustment is a critical component of the revision journey. Patients who have experienced complications or dissatisfaction with their initial FFS may face heightened anxiety, frustration, or even renewed gender dysphoria. The emotional “post-op blues” can be more pronounced, and the process of accepting and integrating a revised self-image can be challenging. Comprehensive pre- and post-operative psychological support is therefore indispensable. Therapists specializing in gender-affirming care can help patients process previous surgical experiences, manage current anxieties, and cultivate realistic expectations for the revised outcome. Support groups with others who have undergone similar journeys can also provide invaluable peer support and a sense of shared experience (Dr. MFO, 2025).
Long-term satisfaction from revision surgery is often high, particularly when patients have a clear understanding of the possibilities and limitations. The ability to address a specific concern that has been a source of distress can lead to a profound improvement in self-confidence and quality of life. Even small, targeted revisions can make a significant psychological impact. However, patients must commit to rigorous post-operative care, including adherence to medication regimens, wound care, activity restrictions, and all follow-up appointments, as this compliance is as crucial for a successful revision as it is for primary surgery (Dr. MFO, 2025).
Ultimately, the revision journey is one of careful consideration, open dialogue, and a partnership between the patient and a highly skilled specialist surgeon. By fostering realistic expectations, prioritizing comprehensive care, and embracing patience throughout the healing process, patients can achieve meaningful and satisfying enhancements that further affirm their authentic selves, even in the face of complex surgical challenges.

Conclusion
Facial Feminization Surgery represents a profoundly impactful and transformative medical journey, offering individuals a critical pathway to aligning their physical presentation with their intrinsic gender identity. The success of FFS is measured not only by its aesthetic outcomes but also by its capacity to enhance psychological well-being, foster social congruence, and significantly improve overall quality of life. While the vast majority of FFS procedures lead to highly satisfying results, an exhaustive and informed understanding of potential complex challenges and their sophisticated management is an essential cornerstone of responsible and expert medical practice.
This comprehensive exploration has systematically dissected the intricate landscape of FFS complications, moving beyond general surgical risks to focus on specific, advanced scenarios. We have illuminated the multifaceted nature of nerve-related issues, detailing the spectrum from temporary sensory alterations to rare instances requiring microsurgical nerve repair. The persistent challenges of edema and seroma have been addressed with emphasis on advanced drainage techniques and specialized compression strategies. Furthermore, we have delved into the complexities of hardware-related complications, bone healing anomalies such as non-union and malunion, and the imperative for surgical debridement and reconstruction in the face of severe or recalcitrant infections. Crucially, the discourse extended to the critical arena of unsatisfactory aesthetic outcomes, underscoring the bespoke nature of revision surgery with advanced techniques like re-osteotomy and judicious fat grafting.
The imperative for advanced diagnostic tools, particularly Cone Beam Computed Tomography (CBCT) and sophisticated 3D planning software, cannot be overstated in this highly specialized field. These technologies enable unprecedented precision in identifying the precise etiology of complications and meticulously pre-planning corrective interventions, thereby mitigating inherent risks and optimizing outcomes. Such technological integration epitomizes the evolution of FFS into a domain characterized by scientific rigor and innovative application.
Central to navigating these complex challenges is the indispensable role of the specialist FFS surgeon. Their profound expertise, honed through extensive experience in both primary and revision gender-affirming facial surgeries, is the bedrock upon which successful complication management rests. This specialization encompasses not only superior technical skill but also a holistic, patient-centric approach that prioritizes comprehensive pre-operative assessment, stringent intraoperative protocols, and empathetic post-operative support. The surgeon’s ability to engage in transparent communication, manage patient expectations, and provide continuous psychological support is as vital as their surgical prowess.
For patients considering or undergoing FFS, particularly those facing the prospect of revision, understanding the journey and cultivating realistic expectations is paramount. The path to resolution, while often highly successful, demands patience, a commitment to rigorous post-operative care, and a robust support system. The psychological adjustment, often an emotional continuum, necessitates readily accessible mental health resources to navigate potential “post-op blues” or lingering dysphoria, ensuring that the transformative physical changes are harmonized with internal well-being.
In conclusion, while FFS offers immense benefits, the readiness to address and expertly manage its complex challenges is a hallmark of advanced surgical care. By prioritizing a multidisciplinary approach that integrates cutting-edge diagnostics, specialized surgical techniques, and comprehensive patient support, the long-term well-being and profound satisfaction of patients can be consistently achieved. This enduring commitment ensures that every individual’s journey toward authentic selfhood is supported with the highest standards of medical excellence and compassionate care, reinforcing FFS as a truly empowering and life-affirming intervention.
What are the most common complex complications in FFS?
Common complex complications can include persistent nerve damage leading to sensory changes, prolonged edema, hardware-related issues such as infection or exposure, bone healing problems like non-union or malunion, and unsatisfactory aesthetic outcomes requiring revision. Infections unresponsive to initial antibiotics may also be considered complex.
How are nerve injuries in FFS typically managed?
Nerve injuries can be managed through various advanced surgical techniques including neurolysis (freeing the nerve from scar tissue), direct microsurgical repair to reconnect severed ends, or nerve grafting where a segment of a less critical nerve is used to bridge a gap. The specific approach depends on the type and severity of the injury.
What diagnostic tools are essential for planning FFS revision surgery?
Essential diagnostic tools include Cone Beam Computed Tomography (CBCT) for high-resolution 3D imaging of bone structures, advanced 3D planning software for virtual surgical simulations, and detailed photographic analysis. For nerve issues, electrodiagnostic studies like EMG and NCS may also be utilized.
What should patients realistically expect from FFS revision surgery?
Patients should realistically expect significant improvement in specific concerns rather than absolute perfection. Revision surgery can correct asymmetries, refine contours, and address functional deficits. However, the presence of scar tissue from previous operations can make healing protracted, and outcomes are optimized with a highly specialized surgeon and diligent post-operative care.
Why is a specialist FFS surgeon crucial for managing complications?
A specialist FFS surgeon possesses an unparalleled understanding of craniofacial anatomy and gender-affirming aesthetics, with extensive experience in revision procedures. This expertise enables accurate diagnosis, sophisticated surgical planning, and precise execution of intricate interventions in altered tissues, minimizing further risks and optimizing complex outcomes.
Bibliography
Dr. MFO. (2025, July 1). FFS Risks: What Transgender Patients Should Know. Dr. MFO – FFS Surgeon in Turkey. https://www.dr-mfo.com/ffs-risks-complications-transgender-patients/
Dr. MFO. (2024, September 16). We asked Dr. MFO: Can FFS go wrong? Dr. MFO – FFS Surgeon in Turkey. https://www.dr-mfo.com/can-ffs-go-wrong/
Facialteam. (2024, October 25). Facial Feminization Surgery Complications: The Risks of FFS. Facialteam. https://facialteam.eu/blog/complications-in-facial-feminization-surgery/
Gender Confirmation Center. (n.d.). Tips for Reducing Risks and Complications Associated With Gender-Affirming Facial Surgery. Gender Confirmation Center. https://www.genderconfirmation.com/ffs-risks-complications/
Hazkour, N., Palacios, J., Lu, W., Goote, P., Rivera, R., & Bastidas, N. (2022). Multiprocedural Facial Feminization Surgery: A Review of Complications in a Cohort of 31 Patients. Journal of Craniofacial Surgery, 33(8), 2502-2506. https://pubmed.ncbi.nlm.nih.gov/36102911/











