As a surgeon dedicated to facial gender affirmation, one of the most frequent and understandable concerns my patients express revolves around the financial aspects of Facial Feminization Surgery (FFS). It’s a complex, life-changing procedure, and navigating the costs in Oregon can feel daunting. This guide aims to demystify the financial landscape of FFS, offering clear, concise answers from a medical perspective, so you can approach your journey with clarity and confidence.

Table of Contents
What Factors Influence the Overall Cost of FFS Surgery in Oregon?
Understanding the comprehensive cost of FFS requires an appreciation of the multifaceted components involved. It’s not simply a “surgical fee.” The total expenditure encompasses several key areas:
Surgeon’s Fee
This constitutes the primary charge for the operative work itself. It directly reflects the surgeon’s expertise, their specialized training in FFS, their reputation, and the complexity of the specific procedures being performed. For instance, a comprehensive FFS, which might include procedures like frontal bone reduction, orbital rim contouring, rhinoplasty, lip lift, and genioplasty, will naturally incur a higher surgeon’s fee than a more limited set of interventions. The surgeon’s fee also accounts for their pre-operative planning, intra-operative execution, and crucial post-operative care.
Anesthesia Fees
Anesthesia is a critical component of any surgical procedure. Anesthesia fees are determined by the type of anesthesia administered (e.g., general anesthesia), the duration of the surgery, and the qualifications of the anesthesia provider (e.g., a board-certified anesthesiologist). Longer and more intricate surgeries will necessitate extended anesthesia time, directly impacting this cost.
Facility Fees
These are charges levied by the surgical facility where the operation takes place. This could be a hospital operating room or an accredited outpatient surgical center. Facility fees cover the use of the operating suite, sterilization of instruments, recovery room services, nursing staff, and essential medical supplies consumed during your procedure. The quality and accreditation of the facility also play a role in this cost.
Pre- and Post-Operative Care
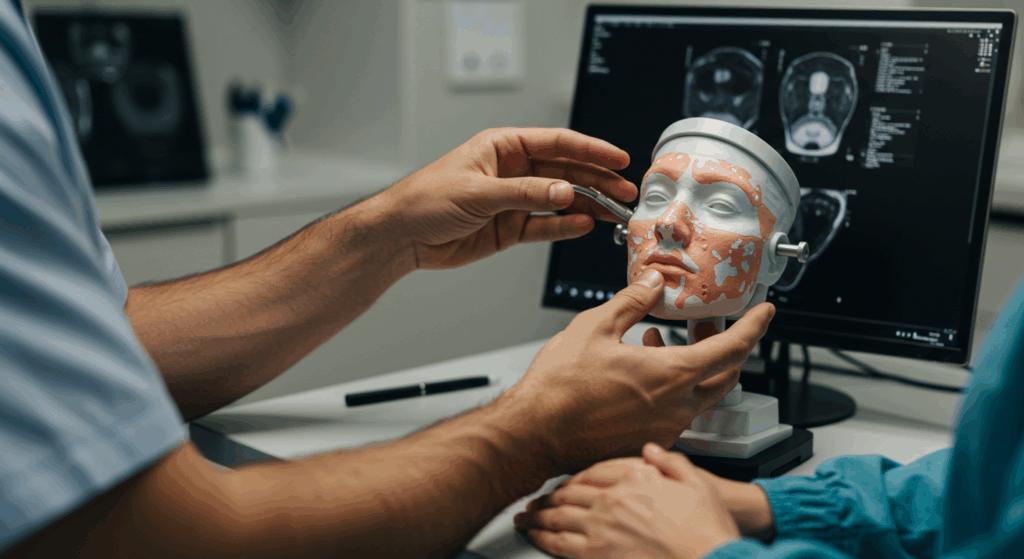
Comprehensive FFS care extends far beyond the operating table. Pre-operative consultations, diagnostic imaging (such as CT scans or X-rays to assess bone structure), laboratory tests, and any necessary medical clearances all contribute to the overall cost. Post-operative care includes follow-up appointments, wound care, and potential management of any post-surgical concerns. While often bundled, it’s important to understand these critical phases.
Ancillary Costs
Beyond the direct medical fees, patients should account for potential ancillary costs. These might include:
- Medications: Prescriptions for pain management, antibiotics, and anti-inflammatory drugs post-surgery.
- Medical Garments: Compression garments or specialized dressings, if required for swelling reduction or healing.
- Travel and Accommodation: For patients traveling to Oregon for surgery, these logistical expenses can be significant.
- Lost Wages: Time off work for recovery should also be factored into your financial planning.
| State | Estimated Cost Range (USD) | Notes |
|---|---|---|
| California | $30,000 – $100,000+ | High-end surgeons, extensive procedure options |
| New York | $25,000 – $90,000 | Premium pricing, top-tier specialists |
| Texas | $20,000 – $75,000 | More affordable options, but limited availability of top-tier specialists |
| Florida | $18,000 – $70,000 | Moderate pricing, some specialized clinics available |
| Illinois | $15,000 – $65,000 | Lower-cost alternatives, fewer surgeons specializing in FFS |
| City | Estimated Cost Range (USD) | Notes |
|---|---|---|
| Portland | $30,000 – $100,000+ | Higher-end surgeons and facilities, extensive procedure options |
| Eugene | $25,000 – $80,000 | Mid-range pricing, fewer specialized surgeons |
| Salem | $20,000 – $70,000 | More affordable options, but limited availability of top-tier specialists |
| Medford | $15,000 – $60,000 | Lower-cost alternatives, fewer surgeons specializing in FFS |
| Bend | $18,000 – $65,000 | Moderate pricing, some specialized clinics available |

Does Insurance Typically Cover FFS in Oregon?
The landscape of insurance coverage for FFS in Oregon is evolving, though it remains highly variable. Historically, many insurance providers classified FFS as “cosmetic” and therefore excluded it from coverage. However, with increasing recognition of gender dysphoria as a medical condition and FFS as medically necessary treatment, more insurance companies are beginning to offer coverage.
Key considerations regarding insurance in Oregon:
- Medical Necessity: The paramount factor for insurance coverage is demonstrating medical necessity. This typically requires a diagnosis of gender dysphoria and letters of support from mental health professionals, affirming that FFS is a medically indicated treatment for your well-being.
- Policy Specifics: Coverage varies significantly between individual insurance plans. It is absolutely crucial to contact your specific insurance provider directly and inquire about their policies regarding gender-affirming care, specifically FFS. Ask about deductibles, co-pays, out-of-pocket maximums, and any pre-authorization requirements.
- In-Network vs. Out-of-Network: Your costs will likely differ based on whether your surgeon and facility are in-network with your insurance plan. Out-of-network providers generally result in higher patient responsibility.
- Prior Authorization: Most insurance companies require prior authorization before approving FFS. This is a meticulous process involving submission of detailed medical records, psychological evaluations, and letters of support to justify the medical necessity of the procedures. Our office staff often assists patients in navigating this complex administrative hurdle.
What is a “Superbill” and How Does it Relate to Reimbursement?
A “superbill” is an itemized form used by healthcare providers to document the services rendered to a patient. It contains all the necessary information for an insurance company to process a claim, including:
- Provider Information: Name, address, and tax ID of the surgeon and facility.
- Patient Information: Your name, date of birth, and insurance policy details.
- Date of Service: When the procedures were performed.
- Procedure Codes (CPT Codes): These are standardized numerical codes that describe the specific medical services performed (e.g., rhinoplasty, brow bone reduction).
- Diagnosis Codes (ICD-10 Codes): These codes explain the medical reason for the services provided (e.g., gender dysphoria).
While we may provide you with a superbill, it’s important to understand that providing one does not guarantee reimbursement. It merely provides the necessary documentation for you to submit a claim to your insurance company for potential out-of-network reimbursement. You would then be responsible for submitting this claim directly to your insurer, and any reimbursement would be paid directly to you. This process can be intricate and often requires persistent follow-up with your insurance provider.
Are There Any Financial Aid Options or Payment Plans Available?
Recognizing that FFS is a significant investment, some patients explore various financial avenues to make surgery more accessible:
- Medical Financing Companies: Several third-party companies specialize in medical financing. These operate much like personal loans, offering various interest rates and repayment terms. It’s crucial to research these options thoroughly and understand all terms and conditions before committing.
- Personal Loans: Banks and credit unions offer personal loans that can be utilized for medical expenses.
- Crowdfunding: Platforms like GoFundMe have become popular for individuals to raise funds from their communities for medical procedures.
- Payment Plans (Limited): While full payment is typically required prior to surgery, some surgical practices or facilities may offer highly individualized payment plans for specific components, but this is rare for the full surgeon’s fee. It is always worth inquiring about any available options during your consultation.
- Grants and Non-Profits: A limited number of non-profit organizations and grants exist to support transgender individuals undergoing gender-affirming surgeries. These are often highly competitive and have specific eligibility criteria. Researching these possibilities can be beneficial, though they are not a primary source of funding for most individuals.
What Happens if I Need Revisional Surgery? Is that an Additional Cost?
While every effort is made to achieve optimal surgical outcomes, it’s critical for patients to understand that revisional surgery is a possibility in any complex aesthetic and reconstructive procedure. The human body heals uniquely, and subtle asymmetries or minor refinements may occasionally be desired or medically indicated after the initial healing period.
- Policy on Revisions: Our practice has a transparent policy regarding revisions. If a revision is deemed medically necessary due to a surgical complication or an outcome that falls outside the expected range based on surgical standards, a portion or all of the surgeon’s fee for the revision may be waived within a specified timeframe. However, facility and anesthesia fees for the revisional surgery would typically remain the patient’s responsibility.
- Patient-Initiated Revisions: If a patient desires a revision purely for aesthetic reasons that fall within the scope of a successful initial outcome, this would typically incur additional fees for the surgeon, anesthesia, and facility, similar to the initial procedure.
During your consultation, we will thoroughly discuss the potential for revisions, our practice’s policy, and how to best prepare for all phases of your surgical journey in Oregon. Our goal is to provide you with the most comprehensive and transparent understanding of FFS, both clinically and financially, ensuring a stress-free planning process as you embark on this transformative path.
Visit Dr.MFO Instagram profile to see real patient transformations! Get a glimpse of the incredible results achieved through facial feminization surgery and other procedures. The profile showcases before-and-after photos that highlight Dr. MFO’s expertise and artistic vision in creating natural-looking, beautiful outcomes.
Ready to take the next step in your journey? Schedule a free consultation with Dr. MFO ( Best Facial Feminization Surgeon for You) today. During the consultation, you can discuss your goals, ask any questions you may have, and learn more about how Dr. MFO can help you achieve your desired look. Don’t hesitate to take advantage of this free opportunity to explore your options and see if Dr. MFO is the right fit for you.
FAQ
How Does the Surgeon’s Experience Impact the Cost?
A surgeon’s fee for FFS is directly correlated with their level of specialized training, years of experience, and established expertise in this highly intricate field. Surgeons who have dedicated their careers to facial gender affirmation, possessing a deep understanding of craniofacial anatomy and a proven track record of successful outcomes, will naturally command a higher fee. This premium reflects not just their time in the operating room, but the extensive pre-operative planning, the precision of their intra-operative techniques, and their commitment to comprehensive post-operative care, all of which contribute significantly to the safety and aesthetic success of your procedure.
Why Are Anesthesia Fees Billed Separately?
Anesthesia services are provided by a distinct medical professional—typically a board-certified anesthesiologist or a certified registered nurse anesthetist (CRNA)—who is not directly employed by the surgical practice. These professionals are responsible for your comfort, vital signs, and overall safety throughout the entire surgical procedure. Their fees are calculated based on the complexity of the anesthesia required and, most importantly, the duration of the surgery. Longer procedures necessitate more extensive monitoring and medication administration, thus increasing the cost associated with this critical aspect of your care.
What Do Facility Fees Cover Beyond the Operating Room?
Facility fees encompass a wide range of services and resources crucial for your surgical safety and recovery. Beyond the use of the sterile operating suite itself, these charges cover the specialized nursing staff who prepare you for surgery, assist during the procedure, and monitor you in the recovery room. They also account for the sophisticated medical equipment, specialized surgical instruments, and all disposable supplies utilized during your FFS. Furthermore, facility fees contribute to maintaining strict accreditation standards, ensuring a safe and compliant environment for complex surgical procedures.
What Types of Pre-Operative Assessments Are Included in the Cost?
Before FFS, a series of comprehensive pre-operative assessments are essential to ensure your readiness for surgery and to meticulously plan the precise surgical approach. These typically include detailed consultations with your surgeon, where your goals are discussed and a physical examination is performed. Often, advanced diagnostic imaging such as high-resolution CT scans of the facial skeleton are required to provide a three-dimensional view of your bone structure, allowing for precise surgical planning. Blood tests and other medical clearances from your primary care physician or specialists may also be necessary to confirm your overall health status and mitigate any potential surgical risks.
How Can Travel and Accommodation Costs Be Managed for Out-of-State Patients?
For individuals traveling to Oregon for FFS, logistical expenses such as travel and accommodation can add a significant layer to the overall cost. To manage these, consider booking flights and lodging well in advance to secure better rates. Research accommodation options near the surgical facility that offer amenities conducive to post-operative recovery, such as accessibility and quiet environments. Some patients also explore extended stay hotels or short-term rental services. Creating a detailed budget specifically for these non-medical expenses, including transportation to and from appointments, can help in stress-free planning.
What Documentation Is Crucial for Insurance Pre-Authorization?
Successfully obtaining insurance pre-authorization for FFS in Oregon hinges on submitting a meticulously prepared documentation package. This typically includes multiple letters of support from licensed mental health professionals confirming a diagnosis of gender dysphoria and articulating the medical necessity of FFS as part of your gender-affirming care. Detailed medical records outlining your gender transition history, any previous hormone therapy, and a comprehensive surgical plan from your FFS surgeon, including specific CPT codes for the procedures, are also paramount. A clear and compelling case for medical necessity, backed by robust documentation, significantly improves the likelihood of approval.
What is the Difference Between In-Network and Out-of-Network Coverage?
The distinction between in-network and out-of-network coverage fundamentally impacts your out-of-pocket costs for FFS. When your surgeon and the surgical facility are “in-network,” they have a contractual agreement with your insurance company to accept a pre-negotiated, discounted rate for their services. This generally results in lower co-payments and deductibles for you. Conversely, “out-of-network” providers do not have such agreements, meaning your insurance will pay a smaller percentage of the total cost, or sometimes none at all, leaving you responsible for a significantly larger portion of the bill. Understanding your specific plan’s benefits for both scenarios is crucial for financial planning.
Why are CPT and ICD-10 Codes Important on a Superbill?
CPT (Current Procedural Terminology) codes and ICD-10 (International Classification of Diseases, Tenth Revision) codes are the standardized language of medical billing, essential for clear communication between providers and insurance companies. CPT codes precisely describe the specific surgical procedures performed (e.g., bone contouring, rhinoplasty), while ICD-10 codes provide the medical diagnosis or reason for those procedures (e.g., gender dysphoria). When correctly applied to a superbill, these codes allow the insurance company to understand exactly what services were rendered and why, enabling them to process claims accurately and determine potential reimbursement for out-of-network services.
How Do Medical Financing Companies Differ from Personal Loans?
While both medical financing companies and personal loans can provide funds for FFS, their structure and focus differ. Medical financing companies, like CareCredit or Alphaeon Credit, are specifically designed for healthcare expenses. They often offer deferred interest or low-interest promotional periods, but strict repayment terms apply. Personal loans, obtained from banks or credit unions, are more general-purpose and typically have fixed interest rates and repayment schedules. The choice depends on your credit score, the interest rates offered, and the flexibility you need for repayment, with medical financing sometimes offering more specialized terms for healthcare costs.
What Constitutes a “Medically Necessary” Revision?
A “medically necessary” revisional surgery is generally defined as one required to correct a functional impairment, address a significant asymmetry that falls outside the expected range of a successful aesthetic outcome, or resolve a complication directly related to the initial surgery (e.g., persistent swelling, minor contour irregularities requiring further refinement). It is not a revision solely for aesthetic preference when the initial result is considered surgically sound. The determination of medical necessity for a revision is made by the operating surgeon based on clinical assessment and adherence to established surgical standards.