Navigating the journey of facial feminization surgery (FFS) is a significant undertaking, marked by careful consideration, research, and, crucially, informed conversations with your surgical team. As a surgeon specializing in FFS, I understand the profound impact these procedures can have on an individual’s life and sense of self. My goal is always to empower my patients with knowledge, ensuring they feel confident and prepared at every stage. This comprehensive guide is designed to address one specific, yet vital, component of FFS: hairline lowering, and the essential questions you, as a prospective patient in the UK, should be prepared to ask during your initial consultation.
A consultation is far more than just a brief chat; it is the cornerstone of a successful surgical outcome. It is your opportunity to articulate your goals, voice your concerns, and gain a deep understanding of the proposed procedures, including hairline lowering. Think of it as a collaborative session where we, as surgeon and patient, establish a shared vision and a realistic plan to achieve it. This detailed exploration will equip you with the medical and technical vocabulary necessary to engage in a meaningful dialogue, while also providing simple explanations to demystify complex concepts.
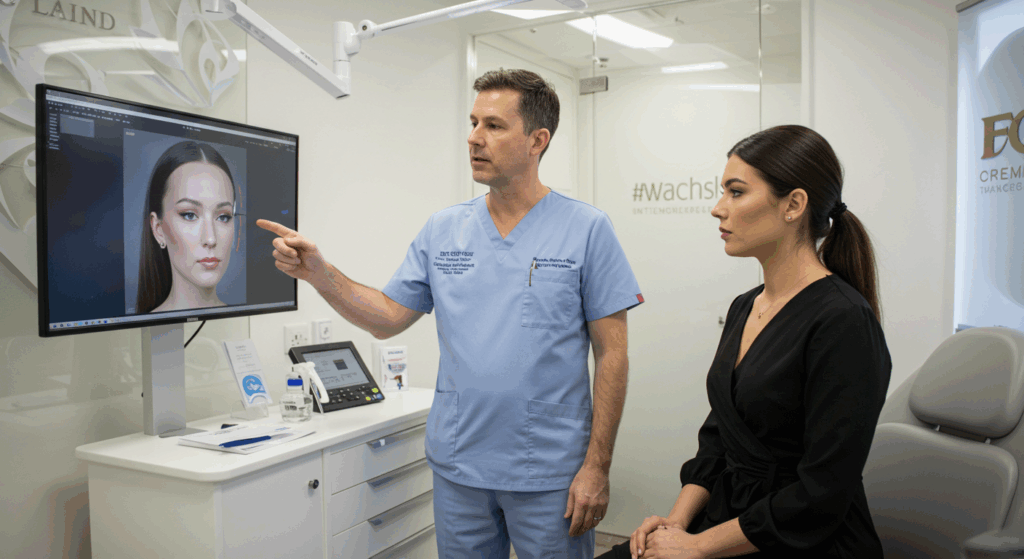
Table of Contents
Understanding Hairline Lowering in FFS
Hairline lowering, medically referred to as a pretrichial forehead reduction or scalp advancement, is a surgical procedure aimed at reducing the vertical height of the forehead. This is achieved by surgically advancing the scalp forward, effectively lowering the hairline to a more aesthetically pleasing and often more feminized position.
Why is Hairline Lowering Considered in FFS?
In the context of FFS, a higher or more traditionally masculine hairline can contribute to a larger-appearing forehead, which may be perceived as a masculine trait. By lowering the hairline, we aim to create a shorter, more rounded forehead, contributing to overall facial harmony and a more feminine aesthetic. This procedure is often performed in conjunction with other FFS procedures, such as forehead contouring (brow bone reduction), brow lift, and rhinoplasty, to address the upper face comprehensively.
The decision to include hairline lowering in your FFS plan depends on several factors, including your existing hairline position, forehead height, scalp laxity (the flexibility and stretchiness of your scalp tissues), and your personal aesthetic goals. During your consultation, we will carefully assess these factors to determine if hairline lowering is the most appropriate approach for you.
The Initial FFS Consultation: Setting the Stage
Your initial consultation is a critical first step. It’s a dedicated time for us to discuss your medical history, understand your motivations for pursuing FFS, and conduct a thorough physical examination. For hairline lowering specifically, I will evaluate your hairline’s shape and position, assess your scalp’s elasticity, and discuss your desired outcome.
This consultation is a two-way street. While I will provide expert assessment and recommendations, it is equally important for you to come prepared with questions. The questions you ask will demonstrate your engagement and help ensure that all your concerns are addressed. They will also help you gauge my experience and approach to hairline lowering surgery.
Crucial Questions to Ask Your Surgeon About Hairline Lowering
Here are some of the most important questions you should consider asking during your initial FFS consultation regarding hairline lowering. I will elaborate on each question, providing the medical context and what you should expect from my response as your surgeon.
Am I a suitable candidate for hairline lowering?
This is arguably the most fundamental question. Your suitability for hairline lowering depends on several anatomical and physiological factors.
Anatomical Considerations:
- Forehead Height: We will measure the vertical distance from the glabella (the smooth area between your eyebrows) to your existing hairline. A forehead height exceeding approximately 5.5 to 6 centimeters is often considered amenable to reduction.
- Scalp Laxity: This is a crucial factor. Scalp laxity refers to how much the scalp can be stretched forward. I will perform a physical assessment to determine your scalp’s elasticity. If you have good scalp laxity, we can achieve a greater degree of hairline lowering in a single procedure. Limited scalp laxity may mean we can only achieve a modest reduction, or it might necessitate a two-stage approach involving tissue expanders.
- Simple explanation: Think of your scalp like a piece of fabric. If it’s very stretchy, we can pull it down quite a bit. If it’s tight, we can only move it a little.
- Hair Density and Quality: The density and quality of your hair along the proposed incision line are important. A dense, healthy hairline helps camouflage the scar effectively.
- Hairline Shape: We will discuss your current hairline shape (e.g., M-shaped, straight, rounded) and how we can reshape it to a more feminine contour.
Physiological Considerations:
- Medical History: We will review your overall health, including any pre-existing medical conditions, allergies, and medications you are taking. Certain conditions can affect wound healing and increase surgical risks.
- Smoking Status: Smoking significantly impairs wound healing and increases the risk of complications such as poor scar healing and skin necrosis (tissue death). I will strongly advise you to stop smoking well in advance of the surgery.
- History of Hair Loss: A history of progressive hair loss, particularly androgenetic alopecia (pattern baldness), needs careful consideration. While hairline lowering can be performed in individuals with a history of hair loss, we need to assess your risk of future hair loss, as significant recession after surgery could expose the scar. In such cases, combining hairline lowering with hair transplantation may be discussed.
My answer to this question will involve a detailed assessment of these factors and a clear explanation of why you are or are not a suitable candidate, along with any potential limitations or alternative strategies.
What specific technique will you use for my hairline lowering?
The primary technique for hairline lowering is the pretrichial incision method. This involves making a surgical incision precisely at the border where the forehead skin meets the hair-bearing scalp.
The Pretrichial Incision:
- Incision Placement: The incision is meticulously designed to follow the natural undulations of your hairline. It is strategically placed so that, as the incision heals, hair follicles can potentially grow through or around the scar, helping to camouflage it.
- Simple explanation: We make the cut right where your hair starts, following the natural edge, so that when it heals, the hair can help hide the line.
- Forehead Skin Excision: A predetermined amount of non-hair-bearing forehead skin is then carefully removed just below the incision line. The amount of skin removed dictates how much the hairline will be lowered.
- Scalp Advancement: The scalp, which is now mobile after the incision, is gently advanced forward and downward to its new, lower position.
- Closure: The incision is then meticulously closed in layers using sutures (stitches) and sometimes staples. The goal is to close the incision with minimal tension to promote optimal healing and minimise scar widening.
Variations and Considerations:
- Incision Pattern: While a relatively straight pretrichial incision is common, some surgeons may use a slightly wavy or “zigzag” pattern. The rationale behind a zigzag incision is that it can potentially lead to a less linear and thus less noticeable scar as it heals. I will explain the specific incision pattern I favour and why, based on your individual hairline and skin characteristics.
- Endoscopic Assistance: In some cases, particularly if a brow lift is also being performed, an endoscope (a small camera) may be used to assist in releasing tissues and facilitating scalp advancement. This is not a separate technique for hairline lowering itself but a tool that can aid in the procedure.
- Tissue Expanders: As mentioned earlier, if scalp laxity is limited and a significant amount of lowering is desired, a two-stage procedure involving tissue expanders may be necessary. In the first stage, a balloon-like device (tissue expander) is surgically placed beneath the scalp. Over several weeks or months, saline solution is gradually injected into the expander, stretching the scalp tissue. Once sufficient laxity is achieved, a second procedure is performed to remove the expander and perform the hairline lowering. I will discuss if this is a consideration in your case.
I will describe the specific steps of the technique I plan to use for your surgery, explaining why it is the most suitable approach based on my assessment of your anatomy and goals.
Where will the scar be located, and how will it be managed?
The primary scar from hairline lowering surgery is located precisely along the new hairline. The goal is to place the incision and manage the healing process in a way that the resulting scar is as inconspicuous as possible, ideally hidden within the hair-bearing scalp.
Scar Location and Appearance:
- Pretrichial Scar: The scar will follow the contour of your new hairline. Immediately after surgery, the incision line will be visible and may appear red or raised.
- Maturation Process: Scars undergo a maturation process over several months, and sometimes up to a year or more. Initially, the scar may be more prominent, but it typically softens, flattens, and fades in colour over time.
- Simple explanation: Scars take time to settle down and become less noticeable, like a new cut that eventually fades.
- Hair Camouflage: A key advantage of the pretrichial incision is the potential for hair follicles adjacent to the incision to grow through or around the scar as it heals. This natural hair growth significantly helps to camouflage the scar.
Scar Management:
- Surgical Technique: Meticulous surgical technique, including precise incision placement and careful closure with minimal tension, is paramount to achieving a fine, well-healed scar.
- Post-Operative Care: You will receive specific instructions on how to care for your incision during the recovery period. This typically involves gentle cleaning and keeping the area dry.
- Scar Massage and Topical Treatments: Once the incision has healed, typically a few weeks after surgery, I may recommend scar massage and/or topical scar treatments, such as silicone-based gels or sheets. These can help soften and flatten the scar.
- Simple explanation: We might recommend gently rubbing the scar or using special creams or patches to help it heal more smoothly and fade better.
- Sun Protection: Protecting the scar from sun exposure for at least a year is crucial, as UV rays can cause the scar to darken and become more noticeable.
- Addressing Scarring Issues: While every effort is made to achieve an optimal scar, sometimes scars can become hypertrophic (raised and thickened) or keloid (growing beyond the original incision boundaries). These are less common with hairline incisions but can occur. If this happens, there are various treatment options, including silicone treatments, steroid injections, and in some cases, revision surgery.
I will show you where the incision will be placed on your forehead and explain the expected appearance of the scar over time, as well as the post-operative care and management strategies to optimise scar healing.
How much can my hairline be lowered?
The extent to which your hairline can be lowered in a single procedure is primarily determined by your scalp laxity.
- Scalp Laxity as the Limiting Factor: As discussed earlier, the more flexible and stretchable your scalp is, the greater the amount of forehead skin that can be removed and the scalp advanced. In individuals with good scalp laxity, it may be possible to lower the hairline by 2 to 5 centimeters, sometimes even more. However, this varies significantly from person to person.
- Desired Aesthetic Outcome: While scalp laxity provides the physical limit, your aesthetic goals also play a role. We will discuss your desired hairline position and how much lowering you hope to achieve, ensuring it aligns with what is realistically possible given your anatomy.
- Assessment During Consultation: During the consultation, I will physically assess your scalp laxity by gently manipulating the scalp. This helps me estimate the amount of lowering that can be safely and effectively achieved in your case.
- Potential for Two-Stage Procedure: If your scalp laxity is limited but you desire a significant amount of lowering, I will discuss the possibility of a two-stage procedure using tissue expanders to gradually stretch the scalp over time before the final hairline lowering surgery.
I will give you a realistic estimate of how much your hairline can be lowered based on my assessment of your scalp laxity and discuss whether a single-stage or two-stage approach might be necessary to achieve your goals.
Will this procedure affect future hair growth?
The pretrichial incision is designed to preserve the hair follicles along the incision line as much as possible. However, there are potential impacts on hair growth that we need to discuss.
Potential Impacts on Hair Growth:
- Temporary Shock Loss: It is common to experience some temporary hair thinning or shedding along the incision line in the weeks to months following surgery. This is known as “shock loss” and is usually temporary, with hair growth typically resuming over several months.
- Simple explanation: Sometimes the hair around the cut gets a bit stressed and falls out temporarily, but it usually grows back.
- Damage to Follicles: While care is taken to preserve follicles, there is a small risk of damage to some hair follicles during the incision and tissue handling. This could result in some permanent thinning along the scar line.
- Scar Alopecia: In rare cases, poor scar healing or excessive tension on the incision can lead to alopecia (hair loss) directly along the scar. This makes the scar more visible.
- Simple explanation: If the scar doesn’t heal perfectly, or if there’s too much pulling on the skin, you might lose some hair right on the scar line.
Mitigating Factors:
- Surgical Technique: A skilled surgeon uses techniques that minimise trauma to the hair follicles during the procedure. Cutting the skin bevelled (at an angle) along the hairline can help preserve more follicles.
- Minimising Tension: Careful closure of the incision with minimal tension is crucial for optimal scar healing and reducing the risk of scar alopecia.
- Addressing Future Hair Loss: If you have a family history or risk factors for progressive hair loss, we will discuss strategies to manage this, which may include medical treatments for hair loss or future hair transplantation to maintain density around the lowered hairline.
I will explain the potential impact on hair growth, the likelihood of temporary shock loss, and the strategies I employ to minimise the risk of permanent hair loss along the scar. We will also discuss your individual risk factors for future hair loss.
What are the potential risks and complications associated with hairline lowering?
Like any surgical procedure, hairline lowering carries potential risks and complications. It is essential that you are fully informed about these before making a decision. While serious complications are uncommon, it’s important to be aware of them.
Potential Risks and Complications:
- Pain and Discomfort: You will experience some pain and discomfort in the forehead and scalp area after surgery, which can be managed with prescribed pain medication.
- Swelling (Oedema) and Bruising (Ecchymosis): Swelling and bruising are expected after surgery and typically subside over several weeks.
- Simple explanation: Your forehead will be puffy and可能有bruises (black and blue marks) after the operation.
- Numbness (Paraesthesia/Dysaesthesia): It is very common to experience altered sensation, including numbness or tingling (paraesthesia), or sometimes an unpleasant or painful sensation (dysaesthesia), in the forehead and scalp after hairline lowering. This is due to the stretching or temporary disruption of sensory nerves during the procedure. Sensation usually gradually returns over several months, but it can take up to a year or more, and in some cases, some degree of permanent numbness or altered sensation may persist.
- Simple explanation: Your forehead might feel numb, tingly, or just plain weird because the small feeling nerves were stretched or bumped during the surgery. This usually gets better over time.
- Scarring Issues: As discussed earlier, issues such as wide or hypertrophic scars, or scar alopecia, are potential complications.
- Infection: Although uncommon, infection at the incision site is a risk with any surgery. Signs of infection include increased pain, redness, swelling, warmth, and pus. Antibiotics may be required.
- Bleeding (Hematoma): Accumulation of blood under the skin (hematoma) can occur, requiring drainage in some cases.
- Poor Wound Healing: Factors such as smoking, poor nutrition, or underlying medical conditions can impair wound healing.
- Nerve Damage: While rare, there is a risk of damage to the frontal branch of the facial nerve, which controls movement of the forehead and eyebrow. Damage to this nerve could result in temporary or, very rarely, permanent weakness or paralysis of the forehead muscles, leading to asymmetry of the eyebrows.
- Simple explanation: There’s a small chance the nerve that helps you raise your eyebrow could be affected, making one side of your forehead hard to move.
- Asymmetry: Achieving perfect symmetry in any facial surgery can be challenging. Minor asymmetries in the hairline position or contour are possible.
- Skin Necrosis: In very rare cases, compromised blood supply to the skin flap can lead to skin necrosis, requiring additional treatment.
- Simple explanation: In extremely rare situations, part of the skin might not get enough blood and could die off.
- Anaesthesia Risks: Risks are also associated with general anaesthesia, although these are rare in healthy individuals.
I will discuss these risks in detail, explaining their likelihood and how I take precautions to minimise them. It is important that you have a realistic understanding of these potential complications.
How do you minimise these risks?
Minimising risks is an integral part of my surgical practice. Several strategies are employed to enhance patient safety and optimise outcomes.
Risk Mitigation Strategies:
- Thorough Pre-operative Assessment: A comprehensive review of your medical history, medications, and lifestyle (including smoking status) helps identify any factors that could increase risks. I may request further tests or consultations with other specialists if necessary.
- Careful Patient Selection: Ensuring that you are a suitable candidate for the procedure based on your anatomy, health, and realistic expectations is the first step in risk reduction.
- Detailed Surgical Planning: Meticulous planning of the incision line, the amount of skin to be removed, and the vector of scalp advancement is crucial.
- Precise Surgical Technique: Using refined surgical techniques, including careful dissection, preservation of blood vessels and nerves where possible, and meticulous closure, helps minimise complications.
- Maintaining Aseptic Technique: Strict adherence to sterile procedures throughout the surgery reduces the risk of infection.
- Avoiding Excessive Tension: Closing the incision without excessive tension is critical for good scar healing and preventing complications like scar alopecia and skin necrosis.
- Post-operative Monitoring and Care: Close monitoring during the immediate post-operative period and providing clear instructions for wound care, activity restrictions, and symptom management helps prevent complications and ensures timely intervention if issues arise.
- Experienced Anaesthesia Team: The procedure is performed under general anaesthesia administered by an experienced consultant anaesthetist who will monitor you throughout the surgery.
I will explain the specific measures I take to minimise each of the potential risks discussed, demonstrating my commitment to patient safety.
What is your experience with hairline lowering surgery?
This is a very important question to ask any surgeon you are considering. Experience matters in complex surgical procedures like hairline lowering as part of FFS.
Assessing Your Surgeon’s Experience:
- Volume of Procedures: Ask how many hairline lowering procedures the surgeon performs annually and how many they have performed in total. A surgeon who performs this procedure regularly is likely to have a refined technique and a better understanding of potential challenges and how to manage them.
- Specialisation in FFS: While many plastic surgeons may perform hairline lowering, a surgeon with a dedicated focus on FFS will have a deeper understanding of the specific aesthetic goals and anatomical considerations relevant to transgender patients.
- Outcomes and Patient Satisfaction: While a surgeon cannot guarantee specific results, you can ask about their typical outcomes and how they measure patient satisfaction.
- Before and After Photos: Reviewing a surgeon’s portfolio of before and after photos of previous hairline lowering patients is crucial. Look for results that align with your own aesthetic goals and observe the scar quality and hairline contour. Pay attention to patients with similar forehead height and hairline characteristics to your own.
I will be transparent about my experience, the number of hairline lowering procedures I have performed, and my approach to achieving natural-looking and satisfying results in the context of FFS.
What happens on the day of surgery?
Understanding the surgical process can help alleviate anxiety. I will walk you through what to expect on the day of your hairline lowering surgery.
The Surgical Day Process:
- Arrival and Admissions: You will arrive at the hospital or surgical centre at the scheduled time and complete the necessary admissions procedures.
- Meeting the Surgical Team: You will meet with the nursing staff, the anaesthetist, and me. This is another opportunity to ask any last-minute questions.
- Pre-operative Marking: I will make markings on your forehead and scalp to outline the planned incision line and the amount of skin to be removed. This is a precise process based on our pre-operative planning.
- Anaesthesia: Hairline lowering surgery for FFS is typically performed under general anaesthesia. This means you will be asleep and pain-free throughout the procedure. The anaesthetist will discuss the anaesthesia process and address any concerns you have.
- Simple explanation: You’ll be completely asleep for the surgery, so you won’t feel anything.
- The Surgical Procedure: Once you are under anaesthesia, the surgical team will prepare the surgical site. I will then perform the hairline lowering procedure as planned, which involves making the incision, removing the excess forehead skin, advancing the scalp, and meticulously closing the incision.
- Duration of Surgery: The duration of the surgery will depend on whether hairline lowering is performed as a standalone procedure or in combination with other FFS procedures. Hairline lowering alone typically takes between 1.5 to 3 hours.
- Recovery Room (Post-Anaesthesia Care Unit – PACU): After the surgery is complete, you will be moved to the recovery room where you will be closely monitored as you wake up from the anaesthesia.
- Transfer to Ward: Once you are stable and fully awake, you will be transferred to a hospital ward for overnight observation, or in some cases, discharged home if it’s a day case and deemed safe.
I will provide a detailed explanation of the surgical day process, ensuring you know what to expect from the moment you arrive until you are in recovery or transferred to the ward.
What is the recovery like after hairline lowering?
Understanding the recovery process is crucial for planning and setting realistic expectations. Recovery from hairline lowering involves several stages, with the initial period requiring the most care and rest.
Immediate Post-operative Period (First few days to a week):
- Pain and Discomfort: You will experience pain and discomfort, which will be managed with prescription pain medication.
- Swelling and Bruising: Significant swelling and bruising in the forehead and around the eyes are expected. Applying cold compresses as instructed can help reduce swelling.
- Numbness: Numbness in the forehead and scalp will be present due to nerve stretching.
- Head Wrap/Dressings: You will likely have a head wrap or dressings in place to help reduce swelling and support the surgical area.
- Drains (if used): In some cases, small drains may be placed under the skin to collect any excess fluid. These are usually removed within a day or two.
- Activity Restrictions: You will need to rest and avoid strenuous activities, bending, and lifting. Keep your head elevated to help reduce swelling.
- Wound Care: You will receive specific instructions on how to care for your incision, which may involve gentle cleaning.
Early Recovery (1 to 3 weeks):
- Swelling and Bruising Subside: Swelling and bruising will gradually subside, although some residual swelling may persist for several weeks.
- Sensation Begins to Return: Sensation in the forehead and scalp may slowly begin to return, accompanied by tingling or itching.
- Return to Light Activities: You can gradually increase your activity level, but avoid anything that significantly increases your heart rate or blood pressure.
- Stitch/Staple Removal: Sutures or staples are typically removed around 7 to 14 days after surgery.
Mid-Term Recovery (1 to 3 months):
- Significant Improvement in Appearance: Most of the swelling and bruising will have resolved, and you will start to see a good indication of your new hairline position.
- Scar Maturation Begins: The scar will still be visible but will begin to soften and fade.
- Sensation Continues to Improve: Sensation will continue to return, although complete return can take longer.
- Return to Most Activities: You can typically return to most normal activities, including exercise, although strenuous activities may still need to be approached gradually.
Long-Term Recovery (3 months and beyond):
- Scar Maturation Continues: The scar will continue to refine and fade over several months.
- Hair Regrowth: If you experienced temporary shock loss, hair growth along the incision line should be well underway.
- Final Results Emerge: The final aesthetic results of your hairline lowering will become more apparent as swelling fully resolves and the scar matures.
I will provide you with a detailed recovery timeline, outlining what to expect at each stage, how to manage symptoms, and when you can gradually resume your normal activities.
When can I return to work and normal activities?
The timeline for returning to work and normal activities varies depending on the individual, the extent of the surgery (whether hairline lowering was performed alone or with other procedures), and the nature of your work or activities.
General Guidelines:
- Light/Sedentary Work: If your job is sedentary and does not involve physical exertion, you may be able to return to work within 1 to 2 weeks after surgery, provided you are feeling well and comfortable.
- Physically Demanding Work: If your job involves physical labour, heavy lifting, or strenuous activity, you will need a longer period of recovery, potentially 3 to 4 weeks or more.
- Strenuous Exercise: Avoid strenuous exercise, including heavy lifting and high-impact activities, for at least 4 to 6 weeks after surgery. Gradually reintroduce exercise as tolerated.
- Social Activities: You may feel comfortable resuming social activities within 2 to 3 weeks, although some residual swelling or bruising may still be visible.
It is essential to listen to your body during recovery and not rush back into activities too soon, as this can compromise healing and increase the risk of complications. I will provide you with personalised guidance on when it is safe for you to return to work and specific activities based on your individual circumstances.
How do I care for the incision site during recovery?
Proper care of the incision site is critical for preventing infection, promoting optimal healing, and minimising scar visibility.
Incision Care Instructions:
- Keeping the Area Clean and Dry: You will receive specific instructions on how to gently clean the incision area. This may involve using a mild soap or saline solution. It is important to keep the incision dry, especially in the initial days after surgery.
- Avoiding Picking or Scratching: Resist the urge to pick at any scabs that form along the incision line, as this can disrupt healing and worsen scarring.
- Managing Itching: Itching along the incision is common as the nerves heal. Avoid scratching. I may recommend over-the-counter or prescription creams to help manage itching.
- Hair Washing: You will be advised on when and how to safely wash your hair after surgery. This usually involves using a gentle shampoo and being careful around the incision.
- Follow-up Appointments: You will have scheduled follow-up appointments so I can monitor your healing, remove sutures or staples, and address any concerns.
I will provide you with detailed written instructions on how to care for your incision, demonstrating the proper techniques for cleaning and dressing changes if required.
When will I see the final results of the hairline lowering?
It is important to understand that the results of hairline lowering, like most surgical procedures, evolve over time. While you will see an immediate change in your hairline position after surgery, the final aesthetic outcome will take several months to become fully apparent.
Timeline for Seeing Results:
- Immediate Post-Surgery: You will see the lowered hairline position immediately after surgery, although swelling and bruising will temporarily obscure the final contour.
- Early Weeks: As the initial swelling and bruising subside over the first few weeks, the new hairline will become more defined.
- Several Months: Over the next few months, the scar will begin to mature and fade, and any temporary shock loss will start to resolve with new hair growth.
- Six Months to a Year: The final results are typically assessed around six months to a year after surgery. By this time, the scar should have matured significantly, and hair regrowth along the incision should be well established, helping to camouflage the scar. The tissues will have settled, and the final hairline contour will be apparent.
It is crucial to be patient during the healing process and understand that the initial appearance is not the final result. I will manage your expectations regarding the timeline for seeing the final outcome and explain the stages of healing.
What results can I realistically expect from hairline lowering?
Managing expectations is a vital part of the consultation process. While hairline lowering can dramatically improve the appearance of a high forehead and contribute significantly to a more feminine facial aesthetic, it is important to have realistic expectations about the degree of lowering achievable, the appearance of the scar, and the overall outcome.
Realistic Expectations:
- Degree of Lowering: As discussed, the amount of lowering is limited by scalp laxity. While significant reduction is often possible, it’s important to understand the realistic range for your individual anatomy.
- Scar Visibility: While the goal is to achieve a well-camouflaged scar, a scar line will be present along the new hairline. In most cases, the scar is inconspicuous and easily hidden by the hair, but its visibility can vary depending on individual healing, hair density, and scar maturation.
- Hairline Shape: We can reshape the hairline to create a more feminine contour, such as a more rounded or oval shape, as opposed to a more traditionally masculine M-shape.
- Overall Facial Harmony: Hairline lowering is often performed as part of a broader FFS plan. The best results are achieved when hairline lowering is integrated harmoniously with other procedures to create overall facial balance and feminization.
- Not a Cure for Hair Loss: Hairline lowering does not prevent future hair loss. If you have a predisposition to pattern baldness, we will need to discuss strategies to manage this.
I will discuss what results are realistically achievable for you based on my assessment of your anatomy, and I will show you before and after photos of patients with similar characteristics to give you a visual representation of potential outcomes. We will also discuss the importance of integrating hairline lowering into your overall FFS goals.
Will I need any follow-up procedures after hairline lowering?
In most cases, a single hairline lowering procedure achieves the desired outcome. However, in some situations, follow-up procedures may be considered.
Potential Follow-up Procedures:
- Revision Surgery: While uncommon, if there are issues with scar healing (e.g., significant widening or hypertrophy) or if minor adjustments are needed to the hairline contour, a scar revision procedure may be considered once the scar has fully matured.
- Hair Transplantation: If you have naturally thin hair along the hairline or experience significant scar alopecia, hair transplantation can be performed to increase hair density and further camouflage the scar. Hair transplantation can be performed as a secondary procedure after hairline lowering.
- Tissue Expansion (if not done initially): If your initial scalp laxity was limited and you desire further lowering, a second stage involving tissue expansion followed by hairline lowering can be performed.
I will discuss the likelihood of needing any follow-up procedures in your specific case based on my initial assessment and your goals.
Can I see before and after photos of your previous hairline lowering patients?
Reviewing before and after photos is an essential part of the consultation process. It allows you to assess the surgeon’s aesthetic style, the quality of their results, and the appearance of the scar in patients with similar characteristics to your own.
What to Look for in Before and After Photos:
- Consistency of Results: Look for a consistent pattern of good outcomes across different patients.
- Scar Quality: Pay close attention to the appearance of the scar along the hairline in the after photos. Look for how well it is camouflaged by the hair.
- Hairline Contour: Assess the shape and naturalness of the lowered hairline.
- Overall Facial Harmony: If hairline lowering was performed as part of a broader FFS, observe how the procedure integrates with other facial features to create overall harmony and feminization.
- Variety of Patients: Ideally, the portfolio should include photos of patients with a range of forehead heights, hair densities, and ages.
I will share a selection of before and after photos of my hairline lowering patients, providing context for each case and highlighting the specific outcomes achieved. These photos are a valuable tool for setting realistic expectations and visualising potential results.
What is the total cost of the hairline lowering surgery?
Understanding the financial aspects of surgery is crucial. The cost of hairline lowering surgery in the UK can vary depending on several factors.
Factors Influencing Cost:
- Surgeon’s Fee: This is the fee for the surgeon’s expertise and time. It varies based on the surgeon’s experience, reputation, and the complexity of the case.
- Hospital/Facility Fee: This fee covers the use of the operating room, equipment, and nursing staff at the hospital or surgical centre.
- Anaesthesia Fee: This fee covers the services of the consultant anaesthetist.
- Pre-operative Tests: You may require some pre-operative blood tests or other investigations, which will have a cost.
- Post-operative Care: Follow-up appointments are typically included in the overall fee, but it’s important to clarify this. Medications and supplies for wound care will be an additional cost.
- Potential for Revisions: It’s important to understand the surgeon’s policy regarding the cost of potential revision surgery if needed.
I will provide you with a detailed breakdown of the estimated costs associated with your hairline lowering surgery, including all anticipated fees. I will also explain what is included in the quoted price.
What is included in the surgical fee?
Clarifying what is included in the fee helps avoid unexpected costs later on.
Typical Inclusions:
- Surgeon’s Fee: The fee for the surgeon’s performance of the procedure.
- Anaesthesia Fee: The fee for the anaesthetist’s services during the surgery.
- Hospital/Facility Fee: Covers the use of the operating room and associated facilities for the duration of the surgery.
- Standard Post-operative Appointments: Most surgeons include a certain number of post-operative follow-up appointments in the overall fee.
Potential Exclusions:
- Pre-operative Tests: Costs for blood work or other necessary tests before surgery.
- Medications: Prescriptions for pain medication, antibiotics, or other drugs needed after surgery.
- Surgical Garments or Supplies: Special dressings or supplies for wound care during recovery.
- Treatment for Complications: Costs associated with treating potential complications, although this can vary depending on the surgeon’s policy and your insurance.
- Revision Surgery: The cost of any subsequent procedures needed to revise the results.
I will provide a clear and comprehensive breakdown of everything that is included in the surgical fee, as well as a list of potential additional costs you should anticipate.
What is your policy on revisions or touch-up procedures?
Understanding the surgeon’s policy on revisions is important, although the goal is always to achieve the desired outcome in the initial surgery.
Revision Policy Considerations:
- Circumstances for Revision: Clarify under what circumstances a revision procedure would be considered (e.g., significant asymmetry, unsatisfactory scar healing).
- Cost of Revision: Understand whether there is a fee for revision surgery and what that fee covers (e.g., surgeon’s fee, facility fee, anaesthesia fee). Some surgeons may offer revision surgery at a reduced fee or without a surgeon’s fee within a certain timeframe if the need for revision is related to the initial surgery’s outcome.
- Timeline for Revision: Discuss the typical timeframe within which revision surgery would be considered after the initial procedure. Scar maturation, for instance, takes time, so revisions for scar appearance would typically not be performed for several months.
I will explain my policy on revision surgery, outlining the conditions under which it would be considered and any associated costs.
What is your cancellation or rescheduling policy?
Unexpected circumstances can arise, so it’s helpful to be aware of the clinic’s policy regarding cancellations or rescheduling.
Policy Details:
- Notice Period: Understand the required notice period for cancelling or rescheduling your surgery without incurring penalties.
- Fees: Inquire about any fees associated with cancellations or rescheduling outside the specified notice period.
- Deposit Policy: Clarify the policy regarding the non-refundable nature of any deposit paid to secure your surgery date.
I will provide you with clear information about the clinic’s cancellation and rescheduling policy.
Beyond the Consultation: Making a Decision and Preparing for Surgery
After your consultation, take time to process the information provided. It is perfectly acceptable to schedule a second consultation if you have further questions or need clarification on any points. Choosing a surgeon for FFS is a significant decision, and you should feel comfortable and confident with your choice.
Making Your Decision:
- Review Your Notes: Go over the information you gathered during the consultation.
- Compare Surgeons (if you consulted with more than one): Consider the surgeon’s experience, approach, the clarity of their explanations, and your comfort level with them.
- Review Before and After Photos: Look at the results again to ensure they align with your aesthetic goals.
- Talk to Former Patients (if possible): Some clinics may be able to connect you with former patients who are willing to share their experiences.
- Trust Your Gut: Ultimately, choose the surgeon with whom you feel most comfortable and confident.
Preparing for Surgery:
Once you have decided to proceed with hairline lowering, you will receive detailed instructions on how to prepare for your surgery. These typically include:
- Medical Clearances: Completing any necessary pre-operative medical tests or obtaining clearance from your GP or specialists.
- Medication Adjustments: Guidance on which medications to stop or adjust before surgery, particularly blood thinners.
- Smoking Cessation: If you are a smoker, reiterating the importance of stopping smoking well in advance of the surgery.
- Arranging for Support: Planning for someone to pick you up after surgery and stay with you for the first 24-48 hours.
- Preparing Your Home: Setting up a comfortable recovery area at home with everything you will need within easy reach.
- Fasting Instructions: Following specific instructions regarding when to stop eating and drinking before surgery.
I will provide you with comprehensive pre-operative instructions to ensure you are well-prepared for your hairline lowering surgery.
Conclusion
Hairline lowering is a powerful procedure that can significantly enhance the feminine appearance of the upper face. By coming to your initial FFS consultation in the UK armed with insightful questions, you empower yourself to make informed decisions about your care. As your surgeon, I am committed to providing you with clear, honest, and comprehensive information, using both medical expertise and simple explanations to ensure you fully understand the procedure, its potential outcomes, and the associated risks.
Your journey is unique, and your consultation should reflect that. Ask the questions that are most important to you, and do not hesitate to seek clarification on anything you do not understand. By working together, we can develop a surgical plan that aligns with your goals and helps you achieve the harmonious and feminized facial features you desire. The path to FFS is one of transformation, and an informed consultation is your essential first step.
Visit Dr.MFO Instagram profile to see real patient transformations! Get a glimpse of the incredible results achieved through facial feminization surgery and other procedures. The profile showcases before-and-after photos that highlight Dr. MFO’s expertise and artistic vision in creating natural-looking, beautiful outcomes.
Ready to take the next step in your journey? Schedule a free consultation with Dr. MFO ( Best Facial Feminization Surgeon for You) today. During the consultation, you can discuss your goals, ask any questions you may have, and learn more about how Dr. MFO can help you achieve your desired look. Don’t hesitate to take advantage of this free opportunity to explore your options and see if Dr. MFO is the right fit for you.










