For many transgender women and transfeminine individuals, the journey toward aligning their physical appearance with their internal identity is one of the most significant endeavors of their lives. It’s a path paved with meticulous research, deep introspection, and profound hope. While Facial Feminization Surgery (FFS) encompasses a suite of procedures, none is perhaps more foundational or impactful than forehead contouring. This isn’t merely about aesthetics; it’s about altering the very structure that most strongly codes a face as masculine in the public eye. It’s about looking in the mirror and finally seeing yourself reflected back.
The forehead is a powerful gender marker. Subconsciously, it’s one of the first features we use to identify gender. For a person experiencing gender dysphoria, this specific area—the brow bone, the slope of the forehead, the position of the eyebrows—can be a constant, painful source of internal dissonance and external misgendering.
This comprehensive guide is written for you, the person who has spent countless hours navigating Reddit forums, watching “FFS Journey” vlogs on YouTube, and scrutinizing before-and-after photos. You are beyond the initial “what is FFS?” stage. You are seeking deep, reliable, and expert-level information to make one of the most important decisions of your life. We will delve into the critical details of transgender FFS for the forehead, exploring the anatomical science, the different surgical techniques, the recovery process, and how to choose a surgeon with confidence. This is not just a medical procedure; it’s the architectural work of realizing your identity.
(Disclaimer: This article is for informational purposes only and is based on extensive research of publicly available medical information, surgical best practices, and patient experiences. It does not constitute medical advice. Always consult with a qualified, board-certified surgeon for personalized medical guidance.)

Chapter 1: The “Why”: Deconstructing Gender Dysphoria and the Forehead
To truly understand the solution, we must first deeply respect the problem. Gender dysphoria related to the face is not vanity. It is a profound and persistent distress stemming from a fundamental incongruence between one’s gender identity and the characteristics assigned to their sex at birth. The forehead and upper third of the face play an outsized role in this distress for several key anatomical reasons.
The Anatomy of a “Gendered” Forehead
When a craniofacial surgeon assesses a forehead for feminization, they are looking at a specific set of scientifically recognized differences that, when taken together, create a distinctly masculine or feminine impression.
- Brow Bossing (Supraorbital Rim): This is the primary culprit. “Brow bossing” refers to the prominent ridge of bone just above the eyes and below the eyebrows. In individuals assigned male at birth, this ridge tends to be much more pronounced, creating a heavier, more hooded appearance over the eyes. This is a direct result of the development of the underlying frontal sinus during a testosterone-driven puberty.
- The Fronto-Nasal Angle and Forehead Slope: Picture a face in profile. In a typical masculine skull, the forehead often has a steeper, more rearward slope from the brow ridge. It can even have a concave appearance above the bossing. In contrast, a typical feminine forehead has a more vertical, rounded, and smoother contour with little to no bossing. The angle where the forehead meets the nose (the fronto-nasal angle) is also generally more open and softer in women.
- Eyebrow Position and Shape: Testosterone influences not just the bone, but the soft tissues as well. Masculine eyebrows tend to be lower, flatter, and positioned directly on or below the brow bone. Feminine eyebrows are typically higher, sitting well above the bone, and often have a more pronounced arch.
- The Frontal Sinus: This is a hollow, air-filled cavity located within the frontal bone, right behind the brow bossing. Its size and position are critically important and are the primary reason why a simple “shave-down” is often insufficient or impossible. The outer wall of this sinus is the very bone that creates the prominent ridge. A surgeon’s entire strategy revolves around the anatomy of this sinus, which can only be properly visualized with a CT scan.
The Psychological and Social Weight of the Brow
These anatomical points are not just clinical observations; they are the source of daily pain for many trans women.
- The Misgendering Trigger: A prominent brow bone casts shadows that can make the eyes appear smaller and deeper-set, a feature often interpreted as masculine. This can lead to being misgendered by strangers, even when all other aspects of one’s presentation are feminine. This single feature can override makeup, hair, and clothing, causing immense frustration and social anxiety.
- The Barrier to “Stealth”: For many (though not all) trans women, the ultimate goal is to navigate the world simply as women, without their trans history being the immediate, defining characteristic of every interaction. This is often referred to as going “stealth.” A masculine forehead can feel like an insurmountable barrier to this goal, creating a constant state of hyper-vigilance and fear for one’s social and even physical safety.
- Internal Dissonance: Beyond how the world sees you, it’s about how you see yourself. Every glance in the mirror, every reflection in a shop window, can be a painful reminder of a feature that feels alien. Alleviating this dysphoria is about achieving peace, reducing the constant mental effort of “looking past” that feature, and finally feeling at home in one’s own face.
Understanding this deep connection between bone structure and identity is why forehead feminization is considered a cornerstone of transgender FFS. It doesn’t just change a feature; it changes how you see yourself and how the world, in turn, sees you.
Chapter 2: The Surgical Blueprint: An In-Depth Guide to Forehead Contouring Techniques
Once you and your surgeon have identified that the forehead is a source of dysphoria, the conversation turns to the “how.” Forehead feminization is a highly technical procedure that requires a craniofacial approach. It is far more complex than simply shaving down bone. The technique chosen depends almost entirely on the degree of your brow bossing and the size and shape of your frontal sinus.
This requires a preoperative CT scan. Let this be an non-negotiable rule: A surgeon who proposes significant forehead contouring without first ordering a CT scan of your skull is not following the highest standard of care. The CT scan is the roadmap that allows the surgeon to see the thickness of the bone, the exact location of your frontal sinus, and plan the surgery safely and effectively.
There are two primary, modern techniques for forehead feminization: Type 1 and Type 3.
The Incision: The Gateway to the Forehead
Before any bone work can begin, the surgeon must gain access to the forehead. This is done via one of two incision types:
- Coronal Incision: This is a classic approach where the incision is made far back on the head, running from ear to ear across the scalp, hidden within the hair.
- Pros: The scar is completely concealed by hair, making it an excellent option for patients who are not concerned about their hairline position.
- Cons: It does not allow for the advancement of the hairline. It also results in temporary (and in rare cases, permanent) numbness of the entire scalp in front of the incision, which can take a year or more to resolve.
- Hairline Incision (Pretrichial Incision): This incision is made along the very front of your hairline.
- Pros: This is the preferred method for most transgender women as it achieves two goals at once: it provides access to the forehead bones and allows the surgeon to physically lower the hairline. A high hairline is another common masculine trait, so advancing it can have a powerful feminizing effect.
- Cons: It leaves a fine scar at the hairline. However, in the hands of a skilled surgeon, this scar is meticulously closed and often becomes nearly invisible over time, especially as hair follicles are sometimes preserved to grow hair through the scar itself.
Technique 1: Type 1 Forehead Contouring (Burring/Shaving)
The Type 1 procedure is the most straightforward but also the most limited. It involves using a surgical burr (akin to a high-speed sander) to shave down the brow bone.
- Who is a candidate? This technique is only suitable for patients with very minimal brow bossing and a very thick anterior wall of their frontal sinus. This is a small minority of FFS patients.
- How it works: The surgeon exposes the bone and simply shaves down the prominence.
- The Critical Limitation: The surgeon can only remove bone until they are just shy of breaching the frontal sinus cavity. If the bossing is created by the sinus bulging outward (which it almost always is), you cannot simply shave it flat without creating a hole into the sinus. Trying to do so would be dangerous and ineffective. For this reason, the Type 1 procedure is not the standard of care for the vast majority of trans women seeking significant feminization. A surgeon who suggests a simple “shave down” for prominent bossing without explaining these limitations should be a red flag.
Technique 2: Type 3 Forehead Contouring (Forehead Reconstruction / Osteotomy & Setback)
The Type 3 procedure is the gold standard for most transgender FFS patients and is capable of producing the most dramatic and natural-looking results. It is a true reconstruction of the forehead. While it sounds complex, it is a safe and well-established craniofacial technique.
- Who is a candidate? Anyone with moderate to severe brow bossing, which encompasses most trans women seeking FFS.
- How it works: This elegant procedure doesn’t just shave the bone; it remodels it.
- Exposure: After the incision, the scalp is carefully lifted to expose the entire forehead bone down to the brow ridge.
- The Osteotomy: The surgeon uses precise instruments to make a very fine cut in the bone around the entire outer wall of the frontal sinus. This piece of bone, known as the “anterior table,” is then carefully removed, like lifting the lid off a box. This provides the surgeon with a clear view of the sinus cavity.
- The Setback: With the bone plate removed, the surgeon can now use a burr to shave down the edges of the sinus opening and the surrounding orbital rims. The bone plate itself is often thinned with a burr. Then, the plate is placed back into position, but now it is “set back” in a flatter, more feminine orientation.
- Fixation: This newly positioned bone plate is securely fixed in place using tiny, medical-grade titanium micro-screws and sometimes small plates. This hardware is biocompatible, generally does not set off metal detectors, and becomes a permanent part of the skull structure.
- Final Contouring: The surgeon then uses a burr to smooth out any remaining steps or irregularities in the surrounding bone, blending the entire forehead into a smooth, harmonious, and naturally feminine curve.
The Type 3 procedure is fundamentally superior for most cases because it is not limited by the sinus. It directly addresses the problem by repositioning the bone itself, allowing for the complete elimination of the brow bossing.
Ancillary Procedures: Completing the Upper Third Feminization
Forehead contouring is rarely performed in isolation. To create a truly harmonious result, it is almost always combined with a brow lift.
- The Brow Lift: Once the underlying bone has been feminized, the eyebrows must be repositioned to match. A masculine brow sits low on the bone, while a feminine brow sits higher. During a brow lift, the surgeon carefully elevates the soft tissues of the brow and anchors them to a higher position. This not only places the brows correctly but also “opens up” the eyes, creating a brighter, more feminine appearance that beautifully complements the newly smooth forehead. The degree of the lift and the final shape of the arch are matters of surgical artistry and are discussed during the consultation.
- Forehead Augmentation: In some, less common cases, a patient may have a flat or concave forehead that requires augmentation rather than reduction. This can be done with biocompatible bone cement (PMMA) or fat grafting to create a rounder, more convex feminine shape. This is sometimes performed in conjunction with a Type 3 reduction to perfect the final contour.
Chapter 3: The Artist and the Architect: Choosing Your FFS Surgeon
The success of your transgender FFS, particularly a complex procedure like a Type 3 forehead reconstruction, hinges almost entirely on the skill, experience, and aesthetic eye of your surgeon. This is one of the most important decisions you will ever make. The anxiety around finding the “right” person and avoiding a “botched” outcome is valid. Here’s how to navigate this process with a clear, analytical mind.
What Defines an Expert FFS Surgeon?
FFS is not a standard cosmetic surgery. It’s a highly specialized sub-field of plastic and maxillofacial surgery. Look for a surgeon who embodies the following:
- Board Certification: They must be board-certified, but in a relevant specialty. The most common backgrounds are Plastic and Reconstructive Surgery or Oral and Maxillofacial Surgery (OMFS), often with additional fellowship training in Craniofacial Surgery.
- Specialization and Focus: Look for a surgeon whose practice is heavily focused on, if not exclusively dedicated to, Facial Feminization Surgery. A general cosmetic surgeon who performs FFS “on the side” may not have the deep, nuanced understanding of the craniofacial anatomy and aesthetic goals specific to trans women. Ask what percentage of their practice is FFS.
- Craniofacial Experience: Forehead reconstruction is a craniofacial procedure. A surgeon’s comfort and experience operating on the bones of the skull is paramount. This is where a background in craniofacial or maxillofacial surgery is a significant asset.
- A Verifiable Track Record: An experienced surgeon will have a large portfolio of before-and-after photos of patients with varying facial structures. Critically, you should ask to see results for patients who had a similar starting anatomy to you.
- The “Aesthetic Eye”: Technical skill is one thing; artistry is another. The goal is not to look “done” or like someone else. The goal is to look like you, but feminized. Review their portfolio. Do their results look natural? Do they achieve harmony and balance, or do the faces look artificial?
The Critical Consultation: Your Vetting Process
The consultation is not just for the surgeon to assess you; it’s for you to interview them. You are in control. Go prepared with a list of detailed questions.
Essential Questions to Ask Your Potential Surgeon:
- “Based on my CT scan, what type of forehead contouring do you recommend for me, and why?” A good surgeon will pull up your CT scan and show you your frontal sinus, explaining exactly why a Type 1 or Type 3 is the appropriate choice.
- “How many Type 3 forehead reconstructions do you perform in a typical month or year?” This speaks directly to their level of experience with the gold-standard procedure.
- “Where will you place my incision, and why do you recommend that location for me?” They should be able to justify a hairline vs. coronal incision based on your specific hairline and goals.
- “What is your approach to the brow lift, and how do you determine the final shape and position?” This reveals their aesthetic philosophy.
- “Can I see multiple before-and-after examples of patients you’ve performed forehead contouring on who had a similar brow structure to mine?” This is the most important evidence you can gather.
- “What are the most common complications you see with this procedure, and how do you handle them?” A surgeon who is transparent about risks is more trustworthy than one who dismisses them.
- “Who administers the anesthesia, and what are their qualifications?” Anesthesia is a critical component of your safety.
- “What does the post-operative care plan look like? How many follow-up appointments will I have?”
Red Flags to Watch For
Your intuition is a powerful tool. If something feels off, it probably is. Be wary of:
- No CT Scan: As mentioned, this is a major red flag for any significant forehead work.
- Vague Answers: A surgeon should be able to answer your technical questions with clarity and confidence.
- High-Pressure Sales Tactics: This is a life-altering medical decision, not a timeshare presentation. You should feel supported, not pressured.
- Unrealistic Promises: No surgeon can promise a “perfect” result or a recovery completely free of pain or swelling.
- Poor Communication: If it’s difficult to get clear information from the surgeon or their office staff before the surgery, imagine what it will be like afterward.
This vetting process, while extensive, is your best defense against a poor outcome. It empowers you to move forward with a sense of security and trust in your chosen surgical partner.

Chapter 4: The Marathon of Healing: A Realistic Recovery Timeline
The surgical theater is where the changes are made, but the healing journey is where they are realized. Social media can sometimes create a distorted picture of recovery, with influencers seeming to bounce back in weeks. The reality is that FFS recovery, especially from forehead work, is a marathon, not a sprint. Understanding this timeline is crucial for managing your expectations and your emotional well-being.
Your journey will be unique, but here is a general, realistic timeline based on the collective experience of thousands of patients.
Phase 1: The Immediate Aftermath (The First 72 Hours)
This is the most intense phase. You will wake up from anesthesia in a recovery room. Your head will be extensively bandaged, often with a compression dressing that wraps around your entire head and under your chin to minimize swelling. You may have a surgical drain placed near the incision to collect excess fluid.
- What to Expect: Significant swelling, discomfort (managed with prescribed pain medication), grogginess, and potential nausea from the anesthesia. The swelling from your forehead will immediately begin to travel downwards due to gravity, so your eyes may start to swell shut.
- Your Job: Rest. Sleep with your head elevated on several pillows to help reduce swelling. Drink fluids and eat soft, simple foods as tolerated.
Phase 2: The Big Unveiling (Week 1)
This week is often the peak of the physical discomfort and swelling.
- What to Expect: Swelling and bruising will likely be at their most dramatic. It’s very common for the bruising to settle around the eyes, giving you two “black eyes.” This is normal. The incision site will be tender. You will likely have a follow-up appointment where your large bandages are removed, and you may graduate to a lighter elastic headband. The surgical drain, if you have one, will be removed.
- Your Job: Continue to rest. Avoid any strenuous activity. Gentle, short walks are good for circulation. Follow your surgeon’s instructions for pain management and incision care precisely. Emotionally, this can be a tough week, as you won’t look anything like your final result. Trust the process.
Phase 3: Turning a Corner (Weeks 2-4)
You’ll start to feel more like yourself again during this period.
- What to Expect: Around the 7-14 day mark, your sutures or surgical staples will be removed. This is a major milestone. Swelling will still be very present, but it will have gone down considerably from its peak. You will start to see the new shape of your forehead emerging, which can be an incredibly emotional and affirming experience. Bruising will fade from dark purple/blue to a more manageable yellow/green.
- Your Job: You can slowly reintroduce more normal activities, but still no heavy lifting or intense exercise. Most people who work desk jobs feel comfortable returning to work (often remotely) around the 2-3 week mark, though you may not feel ready for public-facing roles yet.
Phase 4: The Long Game of Settling (Months 1-6)
This phase is all about patience. The dramatic, acute swelling is gone, but a more subtle, persistent swelling remains.
- What to Expect: The numbness in your scalp will be a dominant feature. It can feel very strange, like you’re wearing a helmet. Tingling or “zapping” sensations are common and are actually a good sign—it means the nerves are beginning to regenerate. The hairline scar will be red and noticeable at first, but it will gradually begin to fade and flatten. You’ll see your results getting better and better with each passing month.
- Your Job: Be patient with your body. Protect your scar from the sun with a high-SPF sunscreen to prevent it from darkening. You can typically resume all normal activities, including exercise, after being cleared by your surgeon (usually around the 6-8 week mark).
Phase 5: The Final Result (1 Year and Beyond)
It can take a full year, and sometimes even up to 18 months, for every last bit of swelling to resolve and for the scar to mature to its final state. The nerves in your scalp can continue to regenerate for up to two years.
- What to Expect: This is when you see the true, final result of your surgery. The bone is healed, the tissues have settled into their new position, and the scar is as faded as it will get. This is the face you will carry forward.
- Your Job: Enjoy your new reality. The constant dysphoria, the social anxiety, the feeling of being in the wrong face—for many, this is when they realize that weight has finally been lifted.

Conclusion: Laying the Foundation for Your True Self
The decision to undergo transgender FFS, and specifically forehead feminization, is a profound act of self-realization. It is a declaration that you deserve to feel at home in your own body, to move through the world with confidence, and to see your true gender identity reflected in the mirror.
We have journeyed through the deep-seated “why” rooted in gender dysphoria, dissected the intricate surgical “how” of Type 1 and Type 3 reconstructions, mapped out a strategy for selecting an expert surgeon, and set realistic expectations for the marathon of recovery.
The key takeaways are clear:
- The forehead is foundational: It is arguably the most critical facial feature for gender recognition.
- Technique matters: A Type 3 reconstruction is the gold standard for most patients, offering the most powerful and natural feminization.
- Expertise is non-negotiable: Your outcome is directly tied to the skill, experience, and artistry of a dedicated FFS surgeon.
- Patience is paramount: Recovery is a long and emotionally complex journey that unfolds over a year or more.
Armed with this knowledge, you are no longer just a hopeful patient; you are an informed advocate for your own health and identity. You have the tools to ask the right questions, to scrutinize the answers, and to choose a path forward that is safe, effective, and aligned with your ultimate goal: to live authentically and to be seen for who you truly are. This is not the end of your journey, but the confident, empowered beginning of its next chapter.
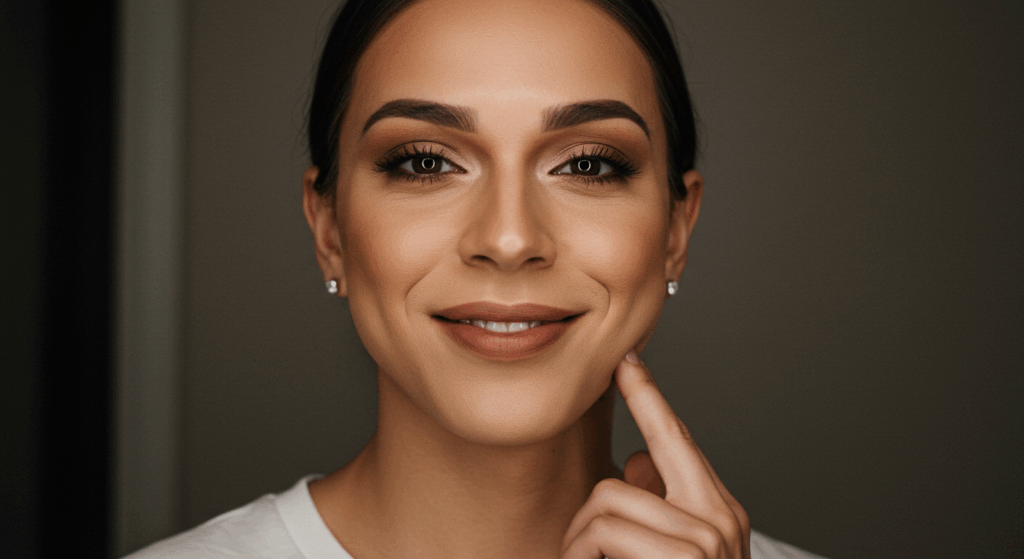
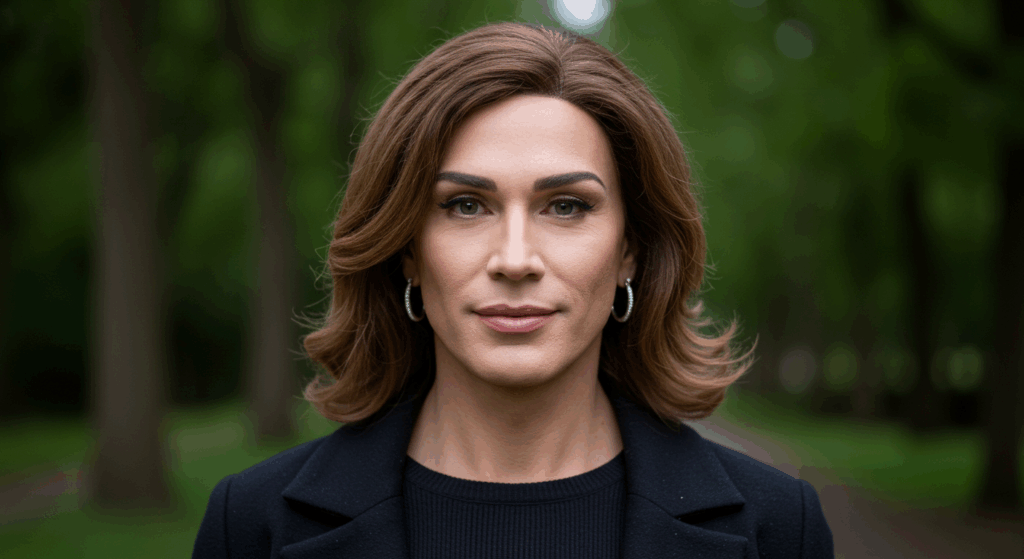
Visit Dr.MFO Instagram profile to see real patient transformations! Get a glimpse of the incredible results achieved through facial feminization surgery and other procedures. The profile showcases before-and-after photos that highlight Dr. MFO’s expertise and artistic vision in creating natural-looking, beautiful outcomes.
Ready to take the next step in your journey? Schedule a free consultation with Dr. MFO ( Best Facial Feminization Surgeon for You) today. During the consultation, you can discuss your goals, ask any questions you may have, and learn more about how Dr. MFO can help you achieve your desired look. Don’t hesitate to take advantage of this free opportunity to explore your options and see if Dr. MFO is the right fit for you.